500 years later, scientists solve Leonardo da Vinci’s heart mystery
In the 16th century, Leonardo sketched the lacy ridges inside the ventricles and guessed they warmed blood in motion.
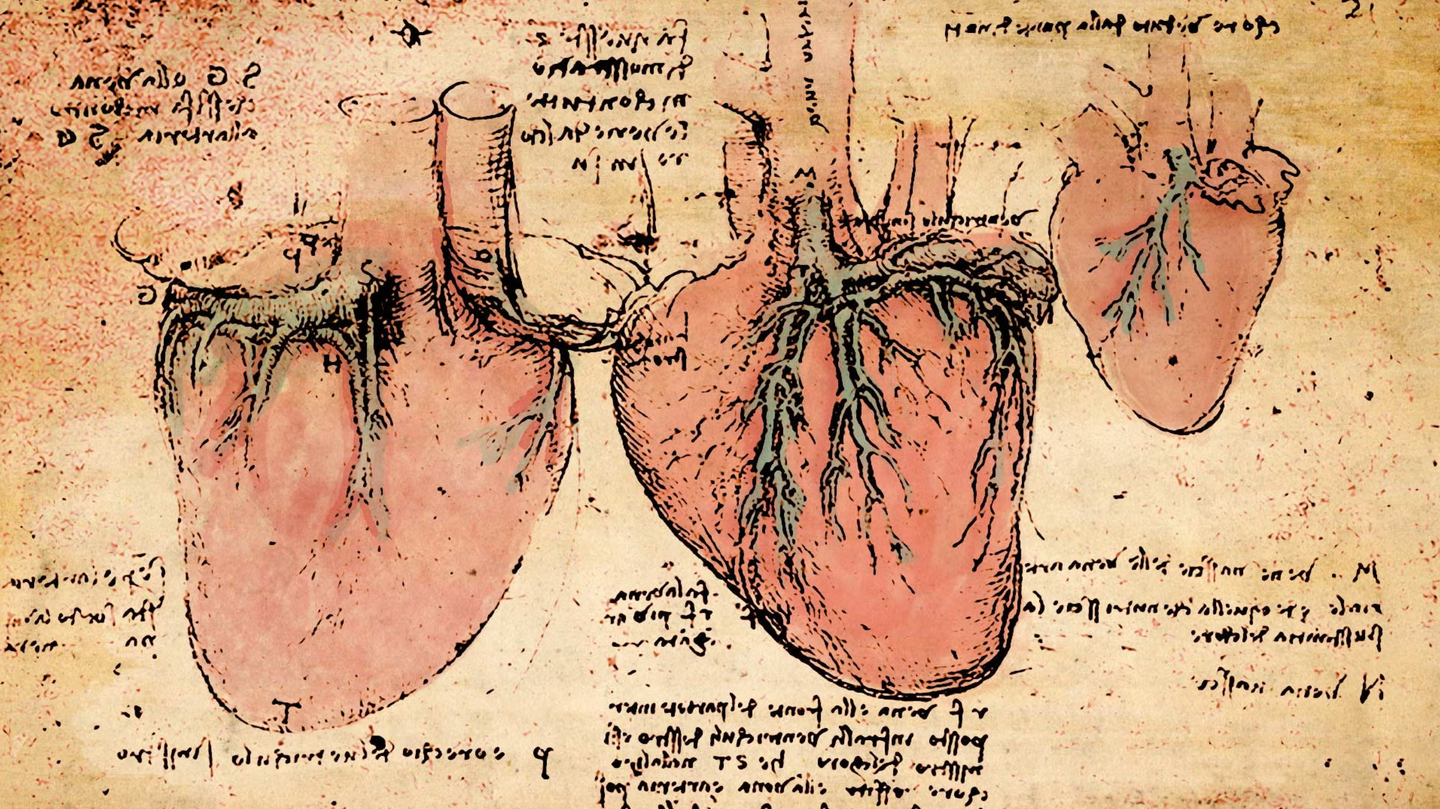
Centuries after Leonardo watched a heart beat, a fresh answer is taking shape. (CREDIT: Leonardo da Vinci / Public domain / Illustration, Ben Wigler)
Centuries after Leonardo watched a heart beat, a fresh answer is taking shape. A new wave of imaging, genetics, and computation shows that the fine mesh of muscle lining the heart—called trabeculae—does more than decorate the ventricles. Its fractal geometry helps move blood and shapes the risk of failure.
The work draws on tens of thousands of MRI scans and large genetic datasets, led by teams at EMBL-EBI, the MRC London Institute of Medical Sciences, Cold Spring Harbor Laboratory, Heidelberg University, and the Politecnico di Milano. The result is a clearer view of how a branching muscle network supports the engine of life.
A 500-year question meets modern data
In the 16th century, Leonardo sketched the lacy ridges inside the ventricles and guessed they warmed blood in motion. Five centuries later, a Nature study put that guess to rest. Investigators applied artificial intelligence to more than 25,000 cardiac MRI scans, then tied the imaging to anatomy and genomics from large cohorts. Their aim was simple but bold: quantify trabecular complexity and ask what it means for flow, pressure, and disease.
They used a measure from geometry called fractal dimension to score the “snowflake-like” branching on the endocardial surface. Those scores linked to heart performance on imaging and to clinical outcomes. In parallel, genome-wide analyses spotlighted genetic regions that tune how the network forms and branches. The team also modeled how fluid moves across a rough inner surface. The simulations lined up with human data: more optimal patterns improve efficiency during filling and ejection, the same way dimples help a golf ball fly farther.
Ewan Birney at EMBL summed up the shift: “Our findings answer very old questions in basic human biology. As large-scale genetic analyses and artificial intelligence progress, we’re rebooting our understanding of physiology to an unprecedented scale.”
How fractal heart trabeculae shape performance
The ventricles do not pump as smooth-walled cylinders. Their inner lining is a textured landscape, built early in development and retained in adult life. That texture expands surface area, shapes vortices, and guides flow. When researchers mapped trabecular geometry across thousands of scans, key patterns emerged. Fractal dimension correlated with stroke work and contractility in biomechanical models and in people. Differences in the branching network also tracked with conduction traits, linking the structure to electrical as well as mechanical behavior.
Related Stories
- Art as medicine: Viewing paintings helps mental health, study finds
- Advanced AI cracks 500 year-old art mystery
The concept is intuitive. A branched surface stirs and streamlines blood within each beat, which can reduce energy loss and help the ventricle fill and eject with less effort. That effect becomes vital as pressure demands rise, or when muscle weakens. In hearts on the edge of failure, small gains in efficiency can matter.
Declan O’Regan, a clinical scientist and consultant radiologist at the MRC London Institute of Medical Sciences, put the work in context. “Leonardo da Vinci sketched these intricate muscles inside the heart 500 years ago, and it’s only now that we’re beginning to understand how important they are to human health. This work offers an exciting new direction for research into heart failure, which affects the lives of nearly 1 million people in the UK.”
Genetic signposts for a branching network
The search did not stop at imaging. Investigators ran large genome-wide association studies using the fractal measure as the trait. They uncovered multiple loci that influence trabecular complexity. Several sit in pathways that regulate actin dynamics and cytoskeletal branching, including genes such as MTSS1 and GOSR2. That makes biological sense. A pathway that sculpts dendrites in neurons can also sculpt the arborization of muscle ridges in the ventricle.
Knockout or knockdown data in animal models supported the picture. When those genes were disrupted, trabecular complexity dropped. In humans, variants that reduce fractal dimension associated with less efficient hearts. As a causal test, Mendelian randomization pointed the same way: reduced complexity nudged risk upward for failure phenotypes. Together, these lines of evidence argue that the network is not a vestige of fetal life, but a working part of the adult pump.
Hannah Meyer of Cold Spring Harbor Laboratory highlighted the team’s blend of tools. “Perhaps even more importantly, we also showed the value of a truly multidisciplinary team of researchers. Only the combination of genetics, clinical research, and bioengineering led us to discover the unexpected role of myocardial trabeculae in the function of the adult heart.”
From patterns to patients
The most immediate clinical question is simple: do trabecular patterns help predict who will develop heart failure? In the large datasets, differences in fractal geometry tracked with incident disease. People with less favorable patterns faced higher risk. Those with richer branching showed protection, even after accounting for common imaging and electrocardiogram measures. That suggests fractal analysis may add value to screening tools now used in clinics.
The work also offers a reason for the mixed signals around “excessive trabeculation.” In some cardiomyopathies, hypertrabeculation appears as a feature on scans. The new data show that context matters. Complexity can be compensatory, harmful, or neutral, depending on the underlying disease process and the rest of the ventricle. A single threshold will not fit all hearts. Instead, a geometry-aware approach—how the network branches and where—can explain why similar-looking scans tell different stories.
What development can teach adult disease
The heart grows trabeculae early, before the coronary vessels deliver oxygen deep into muscle. The high surface area helps diffusion and supports growth. Those ridges also seed conduction pathways that coordinate each beat. Many of the genetic signals tied to adult geometry arise in conserved developmental routes that connect endocardium, myocardium, and matrix. That helps explain why variants in sarcomere genes, which shape muscle assembly, influence trabecular form and function as well.
In brains and hearts, branching raises function by expanding contact and flow across minimal volume. That shared logic suggests deeper links across tissues. Signals that increase dendritic arborization in Purkinje cells, for example, can also increase ridging in a ventricle. When those signals falter, both systems can suffer. Understanding these cross-organ rules could reveal new targets for therapy.
Fractal heart trabeculae in the clinic
Fractal measures are attractive because they can be derived from standard MRI data. With automated tools, a lab can compute a patient’s trabecular profile in minutes. That makes the approach scalable for biobanks and, with validation, for clinics. A geometry score could refine risk in people with borderline measures of function, or in those with genetic variants of uncertain significance. It could also help stratify patients for trials that test drugs or devices aimed at early failure.
Researchers are now pushing in two directions. One is population scale, pulling data from hundreds of thousands of scans to sharpen the links between geometry, genes, and outcomes. The other is mechanism, probing how a ridged surface changes local shear stress, calcium handling, and conduction timing. Both paths will clarify when and how to act on trabecular signals in care.
A multidisciplinary blueprint
The story’s strength is its triangulation. Imaging defined the phenotype. Biomechanics explained why geometry matters. Genetics showed how the pattern forms and how it breaks. Clinical follow-up connected those pieces to risk in the real world. Each method has limits in isolation. Together, they converged on a clear result: trabecular morphology is an important determinant of performance and a contributor to the risk of failure.
That blueprint is reusable. Many organs carry complex internal textures—lungs, intestines, and even the brain’s cortex. With high-throughput imaging and large cohorts, fractal and related measures can reveal how those textures support function and, when perturbed, drive disease.
What comes next
Several gaps need attention. Studies must test whether adding fractal metrics to care improves outcomes, not just prediction. Engineers should refine image processing to handle different scanners and populations. Basic science must trace how shear forces from a rough surface tune cellular responses in endocardium and muscle. And genetic studies in diverse groups are essential, so that risk models work for everyone who needs them.
As those efforts advance, the payoffs could be broad. Screening may get sharper. Therapy could reach patients before they cross the failure threshold. And cardiology will gain a deeper understanding of why hearts with similar ejection fractions behave differently under stress.
Past Studies and Findings
A 2023 study built on the Nature findings by examining trabecular remodeling in a wider set of cardiovascular and muscular conditions. Researchers analyzed imaging and genetic data from diverse patient groups across multiple continents to determine whether fractal heart trabeculae patterns held predictive power outside healthy populations.
They reported that altered trabecular complexity often appeared in individuals with hypertrophic cardiomyopathy, congenital heart defects, and certain muscular dystrophies. In these cases, deviations in trabecular branching patterns were linked to changes in ventricular efficiency, even when standard measures like ejection fraction appeared normal. This suggested that fractal geometry could serve as an early-warning indicator, identifying subtle declines in performance before conventional metrics detect them.
In 2024, follow-up research focused on the genetic architecture of trabeculae across larger and more diverse cohorts, integrating rare variant analyses into the model. This work tied dozens of genes to trabecular form and function, many of which also play central roles in muscle contractility and ventricular wall structure. Notably, researchers highlighted variants in sarcomere-related genes as potential modifiers of trabecular complexity, offering clues about how genetic predispositions might shape both healthy development and disease progression.
The study also demonstrated that adding trabecular complexity scores to existing imaging and ECG-based risk models improved prediction accuracy for heart failure and arrhythmias, further supporting the clinical utility of incorporating fractal-based measures into routine cardiac assessment.
Practical Implications of the Research
Clinicians could add fractal metrics to routine MRI reads to refine risk in borderline cases and to flag patients who need closer follow-up. Because the measure is automated and derived from existing scans, it can scale without major new equipment.
Researchers can use fractal scores as end points in trials that test therapies intended to support ventricular efficiency. If a drug or device improves trabecular flow dynamics or preserves geometry under stress, the fractal dimension may capture that early.
Genetic insights open a path to targeted interventions. If variants in actin-regulating pathways shape trabecular branching, small molecules that modulate those pathways could help maintain performance in vulnerable hearts. Developmental signals that govern early ridging may also be tuned to prevent maladaptive remodeling in disease.
Population health may benefit as well. Large, diverse biobanks can help build risk models that work across ancestries and ages. With those models in hand, health systems could focus prevention on the people most likely to progress to failure.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.