AI tool predicts brain tumors before surgery with near-perfect precision
New AI system identifies brain tumors before surgery with over 97% accuracy, helping surgeons plan care more safely.

 Edited By: Joseph Shavit
Edited By: Joseph Shavit
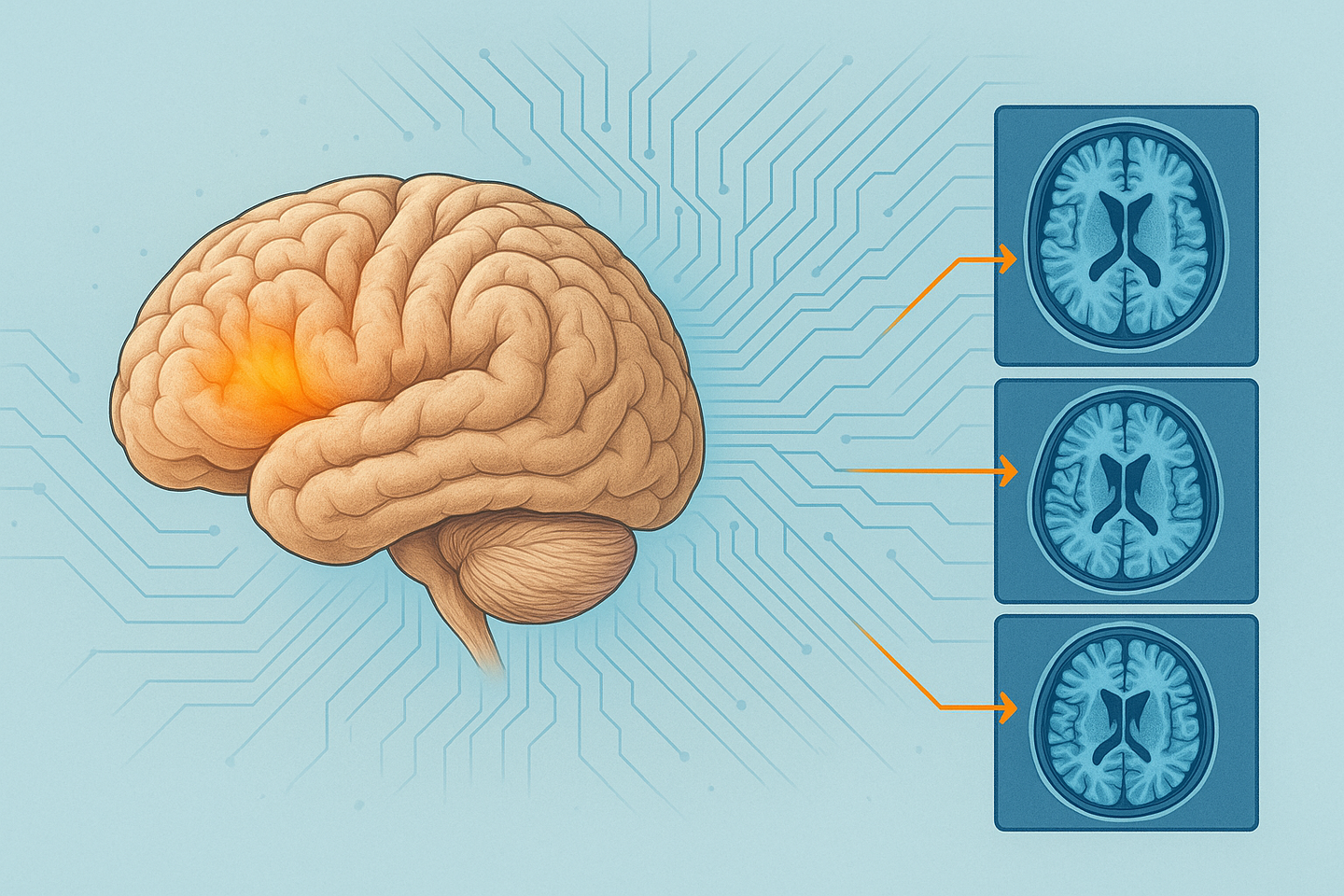
A new AI tool from Thomas Jefferson University can identify two similar brain tumors using routine MRI scans, improving surgical planning and patient safety. (CREDIT: AI-generated image / The Brighter Side of News)
A routine brain scan can look clear but still leave surgeons guessing. Two benign tumors near the pituitary gland often appear nearly identical on MRI. Choose the wrong one, and the entire surgical plan can change. Now, a new artificial intelligence system from Thomas Jefferson University promises to remove much of that doubt before a patient ever enters the operating room.
The research team developed an automated machine learning, or AutoML, program that separates pituitary macroadenomas from parasellar meningiomas using standard MRI scans. The findings, reported in Otolaryngology–Head and Neck Surgery, mark the first time this type of technology has been used to tell these two growths apart before surgery.
Pituitary macroadenomas grow from the hormone-making gland at the brain’s base. Parasellar meningiomas arise from the tissue surrounding that area. Both can press on optic nerves, blood vessels, and vital brain structures. Because each tumor calls for a different surgical approach, an early and accurate diagnosis can guide how surgeons enter the skull and what outcome they can promise.
“Our automated machine learning model achieved over 97% accuracy in distinguishing between two common types of skull base tumors using preoperative MRI scans,” said Gurston G. Nyquist, MD, a professor of otolaryngology and neurological surgery who led the work. “This work is significant because it demonstrates that automated machine learning can streamline model development for medical imaging classification, reducing barriers to implementing artificial intelligence-based diagnostic support in otolaryngology.”
Nyquist added that the system could assist hospitals of all sizes. “While multi-institutional validation and careful integration into clinical workflows are warranted,” he said, “this study represents an important step in the development of reliable tools that may improve skull base tumor diagnosis in both community and tertiary care settings.”
Why an early answer matters
Unlike many cancers, these brain tumors are not usually biopsied before surgery. Doctors must rely on imaging alone to decide what they are dealing with. Even seasoned specialists can disagree. According to the study authors, accuracy in reading scans for this region ranges from about 83% to nearly 97%, depending on training and experience.
When a scan leads doctors astray, the impact is felt in the operating room. A surgeon might take a longer route than needed, expect to remove more tumor than is safe, or underestimate risks tied to blood vessels. Extra tests and second opinions can also delay care and increase stress for families.
The new system aims to sharpen that first judgment. AutoML automates many technical steps that usually require deep coding skills. In this project, the program learned to detect subtle image patterns that people struggle to measure in a consistent way. It does not replace a doctor’s eye. It adds another perspective that never tires.
What the numbers show
To train the model, the team used 1,628 MRI images from 116 patients. At standard settings, the system correctly classified tumors 97.55% of the time. For pituitary macroadenomas, it reached 97% sensitivity and 98.96% specificity. Sensitivity reflects how well true cases are found. Specificity shows how often false calls are avoided. For parasellar meningiomas, sensitivity stood at 98.41% and specificity at 95.53%.
The researchers then tested the model on 959 new images it had never analyzed. The accuracy held steady. That external test is essential before any tool can be trusted in clinics.
Another feature gives physicians control. Hospitals can adjust confidence thresholds after the model is built. A setting that favors sensitivity can reduce the risk of missing a case. A setting that favors specificity can limit unnecessary alarms. This tuning lets the same program serve different needs.
Changing daily care
In smaller hospitals, where skull base specialists may not be available, the high-sensitivity setting could reach 99.39%. That may help staff decide when to seek expert input early. In major centers that see many complex cases, a high-specificity mode has tested as high as 99.31%. That could cut down on false leads and wasted time.
The team sees the tool supporting early triage, training young doctors to recognize patterns, and helping surgeons prepare for what lies ahead. A better plan before incision often means a smoother operation and a safer recovery.
Researchers also want to expand the tool’s reach. Plans include adding other scan types and clinical details, such as hormone levels, that offer clues beyond images. Another goal is teaching the system to identify more than one condition at a time when needed. Future projects may apply the same approach to thyroid growths and voice-box exams.
For now, attention remains on testing the system across many hospitals and fitting it into daily routines. The researchers stress that any digital aid must work quietly in the background and support, not disrupt, patient care. Doctors will still make the final call.
For those facing brain surgery, a clearer label before the operation can bring calmer expectations. A more accurate scan reading may not remove fear, but it can replace guesswork with facts.
Practical Implications of the Research
This technology could shorten the time between a scan and a treatment plan. Patients may receive clearer explanations and fewer last-minute changes in strategy. Hospitals without specialist teams could benefit from expert-level support at the point of care.
Over time, the approach may lower costs by reducing extra tests and repeat operations. The model may also train future doctors to recognize difficult cases sooner.
As it expands to other conditions, artificial intelligence could become a silent partner in daily diagnosis.
Research findings are available online in the journal Otolaryngology.
Related Stories
- AI breakthrough detects brain tumors the size of a pinhead with 97% accuracy
- AI technology identifies cancerous brain tumors in seconds
- FDA-approved antidepressant shown effective at treating brain tumors
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Shy Cohen
Writer



