Breakthrough discovery could reduce the effects of Alzheimers disease by 80%
Compelling evidence suggests that the misfolding, aggregation, and cerebral deposition of amyloid-beta (Aβ) plays a big role in the disease

[July 16, 2023: Caitie Barkley, University of Texas Health Science Center at Houston]
A novel, disease-modifying therapy for Alzheimer’s disease may involve the whole exchange of blood. (CREDIT: Creative Commons)
Alzheimer’s disease (AD) is the major form of dementia in the elderly population. The main neuropathological changes in AD patients are neuronal death, synaptic alterations, brain inflammation, and the presence of cerebral protein aggregates in the form of amyloid plaques and neurofibrillary tangles.
Compelling evidence suggests that the misfolding, aggregation, and cerebral deposition of amyloid-beta (Aβ) plays a central role in the disease. Thus, prevention and removal of misfolded protein aggregates is considered a promising strategy to treat AD.
A novel, disease-modifying therapy for Alzheimer’s disease may involve the whole exchange of blood, which effectively decreased the formation of amyloid plaque in the brains of mice, according to a new study from UTHealth Houston.
A research team led by senior author Claudio Soto, PhD, professor in the Department of Neurology with McGovern Medical School at UTHealth Houston, in collaboration with first author Akihiko Urayama, PhD, associate professor in the department, performed a series of whole blood exchange treatments to partially replace blood from mice exhibiting Alzheimer’s disease-causing amyloid precursor proteins with complete blood from healthy mice of the same genetic background. The results of the study were published in Molecular Psychiatry.
Related Stories
“This article provides a proof-of-concept for the utilization of technologies commonly used in medical practice, such as plasmapheresis or blood dialysis, to ‘clean’ blood from Alzheimer’s patients, reducing the buildup of toxic substances in the brain,” said Soto, director of the George and Cynthia Mitchell Center for Alzheimer’s Disease and Related Brain Disorders and the Huffington Foundation Distinguished Chair in Neurology at McGovern Medical School. “This approach has the advantage that the disease can be treated in the circulation instead of in the brain.”
Previous studies by Soto and other UTHealth Houston researchers have shown that the misfolding, aggregation, and buildup of amyloid beta proteins in the brain plays a central role in Alzheimer’s disease. Therefore, preventing and removing misfolded protein aggregates is considered a promising treatment for the disease.
However, the treatment of Alzheimer’s disease has long been complicated, due to the difficulty in delivering therapeutic agents across the blood-brain barrier. Through their latest research, Urayama, Soto, and others discovered that manipulating circulating components in Alzheimer’s disease could be the key to solving this issue.
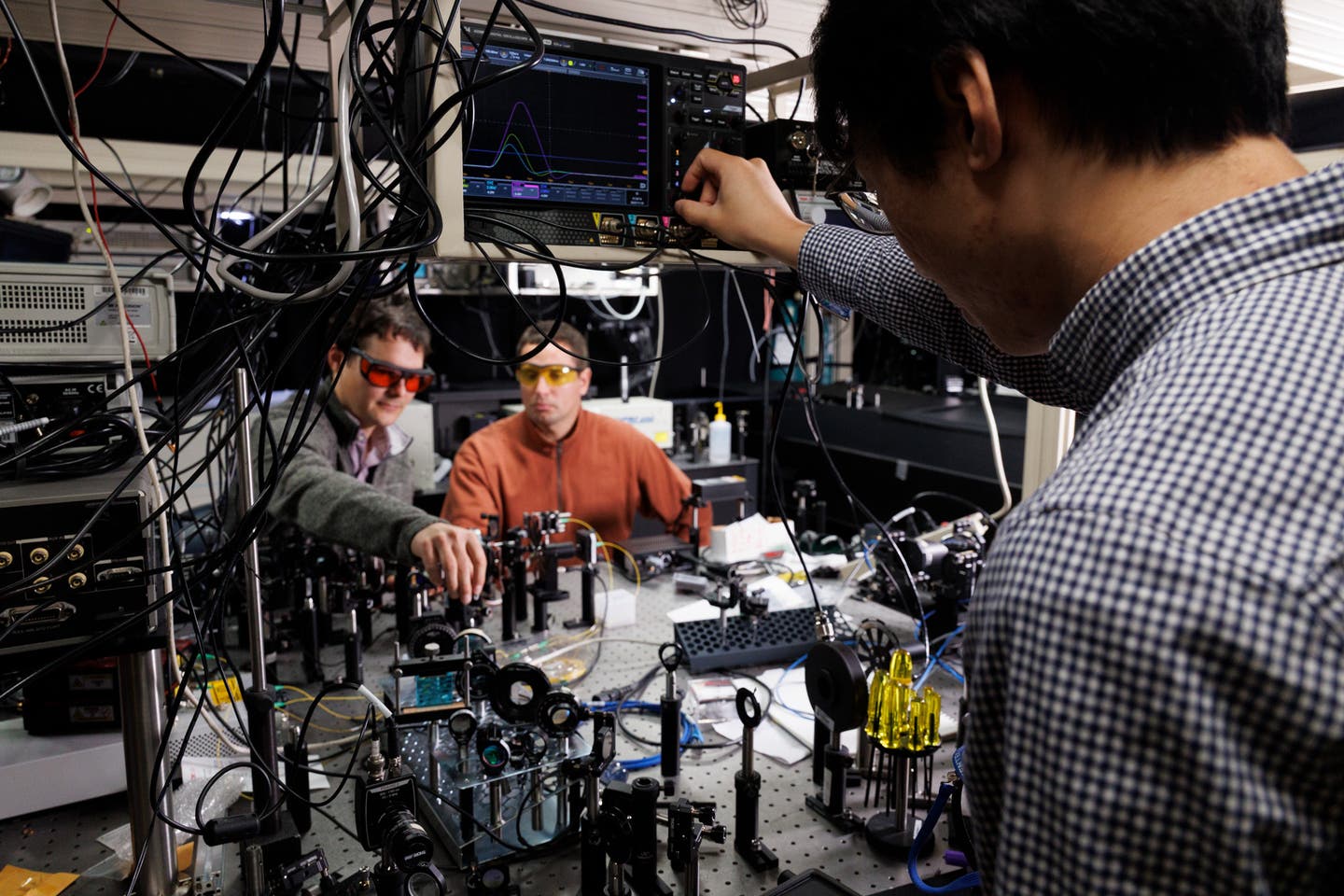
A team led by Claudio Soto, PhD, performed a series of whole blood exchange treatments to partially replace blood from mice with Alzheimer’s disease-causing amyloids in their brains with blood from healthy mice. (CREDIT: UTHealth Houston)
“Blood vessels in the brain are classically considered the most impermeable barrier in the body,” Urayama said. “We have been aware that the barrier is at the same time a very specialized interface between the brain and the systemic circulation.”
After multiple blood transfusions, the researchers found that the development of cerebral amyloid plaques in a transgenic mice model of Alzheimer’s disease was reduced by 40% to 80%.
Schematic representation of the sites used for blood exchange along the jugular brain. C: Simulation curves to estimate the percentage of blood replacement considering the bodyweight of animals and the volume of blood withdrawal. (CREDIT: UTHealth Houston)
This reduction also resulted in improved spatial memory performance in aged mice with the amyloid pathology, and lowered the rates of plaque growth over time.
The exact mechanism by which blood exchange reduces amyloid pathology and improves memory is presently unknown, but measurements of Aβ in plasma soon after blood exchange suggest that mobilization of Aβ from the brain to blood may be implicated.
Our results suggest that a target for AD therapy may exist in the peripheral circulation, which could open a novel disease-modifying intervention for AD.
One possible explanation is that lowering amyloid beta proteins in the bloodstream may help facilitate the redistribution of the peptide from the brain to the periphery.
Blood exchange treatment scheme. A: Schematic representation of blood withdrawal and infusion procedure. In Tg2576 mice at the age of 3 through 17 months. (CREDIT: UTHealth Houston)
Another theory is that blood exchange somehow prevents amyloid beta influx, or inhibits the re-uptake of cleared amyloid beta, among other potential explanations.
However, regardless of the mechanisms of action associated with the blood exchange treatment, the study shows that a target for Alzheimer’s disease therapy may lie in the periphery.
Note: Materials provided above by University of Texas Health Science Center at Houston. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.