Antimalarial drug could treat cystic fibrosis, Duchenne muscular dystrophy, as well as some cancers
Malaria drug mefloquine may boost genetic disease therapies by helping ribosomes ignore faulty stop signals in DNA.

New research shows malaria drug mefloquine can help existing treatments for genetic diseases like DMD work better, with fewer side effects. (CREDIT: CC BY-SA 4.0)
In many genetic diseases, a small error in the DNA code can have devastating effects. These errors, called nonsense mutations, insert a premature stop signal in the genetic instructions that cells use to make proteins. As a result, the cell produces only a short, useless fragment of the needed protein. Without the full protein, essential body functions break down.
This kind of error appears in a wide range of diseases, including some cancers and inherited disorders like Duchenne muscular dystrophy (DMD). Unfortunately, there are few treatments for these conditions. But new research is bringing hope by exploring how certain drugs can help cells ignore these faulty stop signs and produce complete, working proteins.
The Challenge of Nonsense Mutations
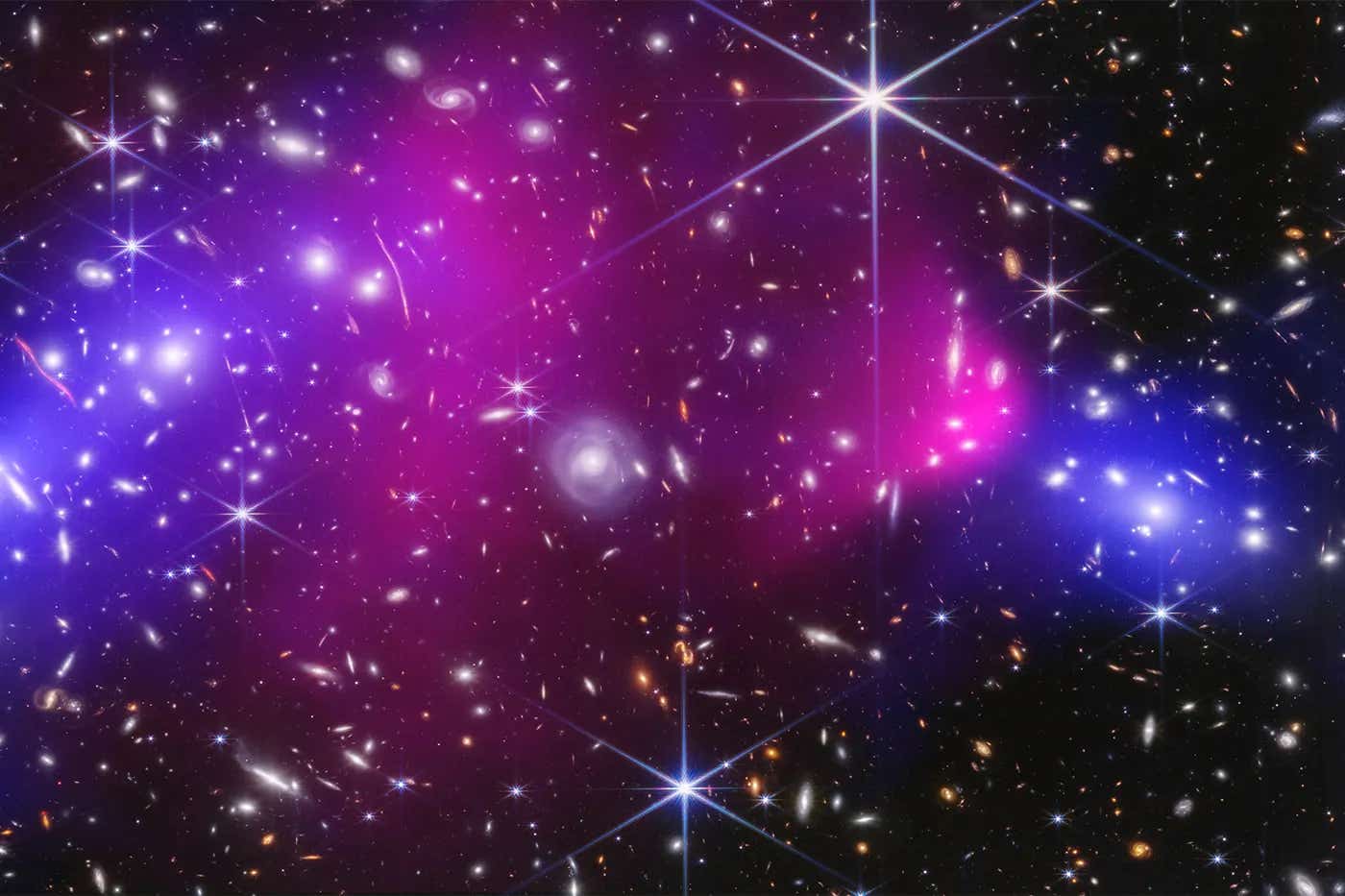
Proteins are built by ribosomes, the tiny molecular machines inside cells. Ribosomes read the genetic instructions and assemble amino acids into proteins, like following a recipe step by step. When a nonsense mutation inserts a stop codon in the wrong place, it’s like slamming the brakes halfway through the recipe. The ribosome stops too soon, leaving the protein incomplete.
Aminoglycosides, a class of antibiotics, were the first drugs found to help ribosomes read past these incorrect stop signals. But they come with a serious catch: high doses are needed to work, and those doses often cause side effects like kidney damage and hearing loss. This makes them risky for long-term use, especially in children or those already battling chronic illness.
A Surprising Partner: Mefloquine
Now, an international team of scientists has discovered that another drug—mefloquine—could make aminoglycosides much more effective, even at lower doses. Originally used to fight malaria, mefloquine has now been shown to help ribosomes override faulty stop codons more efficiently.
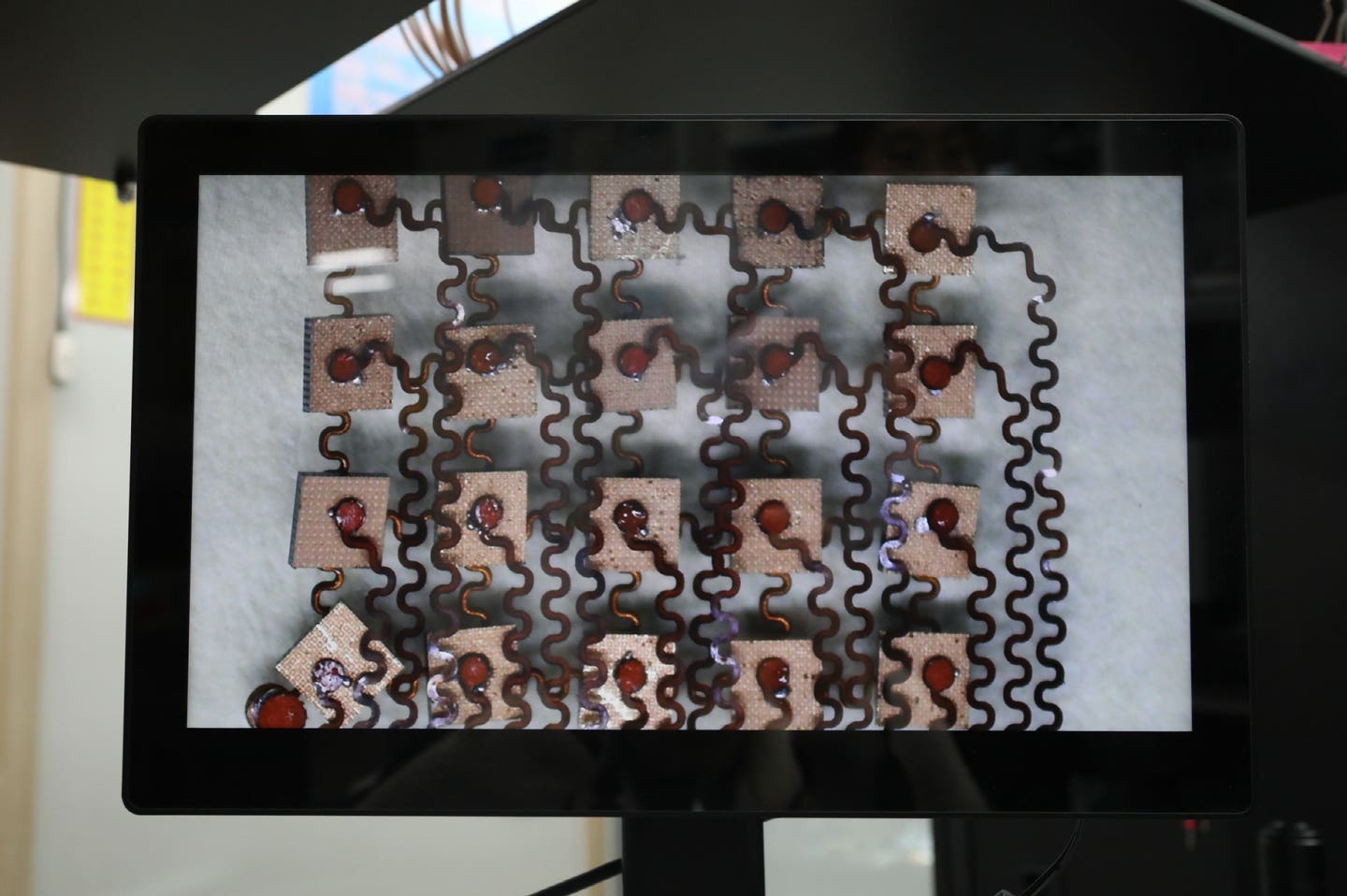
The study, published in Proceedings of the National Academy of Sciences, was led by Dr. Albert Guskov at the University of Groningen. Using X-ray crystallography and cryogenic electron microscopy, his team captured detailed images of how mefloquine and aminoglycosides interact with the ribosome. These tools allowed the researchers to see where the drugs bind and how they change the ribosome’s behavior.
Related Stories
What they found was unexpected. Mefloquine binds near a part of the ribosome known as bridge B7b/c. This area is crucial for the ribosome’s subunits to rotate and function properly during protein production. When mefloquine binds here, it alters the dynamics of these movements. This shift makes it easier for aminoglycosides to encourage the ribosome to read through the incorrect stop codon and continue building the full-length protein.
“It was exciting to discover something completely unexpected,” said Dr. Guskov. “A new mechanism that explains how drugs can help override a faulty stop signal. A very thrilling and motivating discovery.”
Promising Impact on Duchenne Muscular Dystrophy
One of the diseases that could benefit most from this finding is Duchenne muscular dystrophy, or DMD. This condition affects mostly boys and causes progressive muscle weakening, often leading to early death. About 10% to 15% of DMD cases are due to nonsense mutations.
Right now, patients with this form of DMD have limited options. Aminoglycosides like gentamicin and therapies like Translarna have been tried, but their side effects and inconsistent success limit their use.
By adding mefloquine to the mix, doctors might be able to reduce the dose of aminoglycosides needed. That would mean fewer side effects, which could open the door for longer and safer treatment. Even more importantly, mefloquine could help ribosomes produce full-length dystrophin—the key protein missing in DMD. Restoring this protein could improve muscle strength and slow disease progression.
Expanding Possibilities Beyond Muscle Disease
Although DMD was a key focus, the potential uses of mefloquine may stretch far beyond. Since nonsense mutations play a role in many genetic disorders, including cystic fibrosis and some cancers, this discovery could impact many lives.
The fact that mefloquine is already approved by the FDA for malaria adds another advantage. Its safety profile is well understood, so researchers may be able to move more quickly toward clinical trials for its new use. This could save years of testing and approval time.
Still, more work needs to be done. The recent findings were made using ribosome structures, not in living cells or patients. The next step is to study how this combination therapy works in animals and, eventually, in human trials. Researchers also hope to design new drugs that copy mefloquine’s effects but with even fewer side effects or better targeting.
The Road Ahead: Safer and Stronger Treatments
This discovery is not just about adding another drug to a treatment plan. It’s about understanding how the drugs work at a deep, molecular level. Knowing exactly where and how mefloquine binds to the ribosome gives scientists a map. That map can be used to design better therapies—ones that deliver the same benefits with more precision and less harm.
The research also suggests a broader principle: read-through of premature stop codons isn’t just about tricking the ribosome. It involves shifting its internal dynamics—how it moves, rotates, and interprets genetic instructions. By targeting those dynamics, scientists can potentially create more effective treatments not just for DMD, but for a host of genetic diseases.
This kind of insight is what turns basic research into real-world medicine. As more is learned about the ribosome’s behavior, the hope is that new therapies will be safer, more reliable, and available to more patients sooner.
For now, the combination of aminoglycosides and mefloquine offers a fresh path forward. It’s a reminder that sometimes, drugs built for one purpose—like fighting malaria—can find a new and powerful use in an entirely different battle.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.