Australian scientists find potential cure for diabetes, study finds
Scientists at the Baker Heart and Diabetes Institute have made significant strides towards regenerating insulin in pancreatic stem cells.
[Jan. 8, 2024: JD Shavit, The Brighter Side of News]
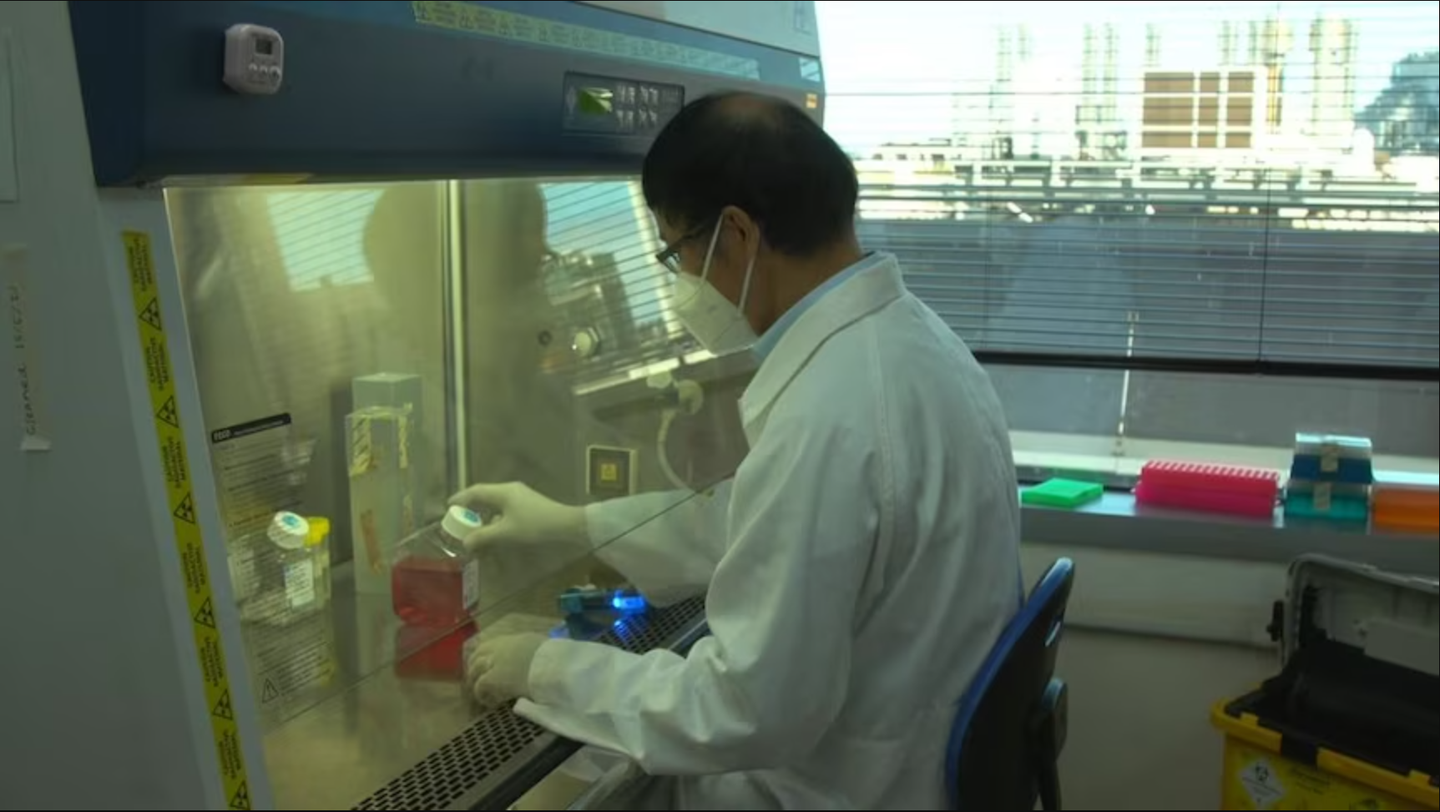
Scientists at the Baker Heart and Diabetes Institute have made significant strides towards regenerating insulin in pancreatic stem cells. (CREDIT: Baker Heart and Diabetes Institute)
In an exciting development in the field of diabetes research, scientists at the Baker Heart and Diabetes Institute have made significant strides towards regenerating insulin in pancreatic stem cells, potentially eliminating the need for regular insulin injections.
Their groundbreaking findings, published in the prestigious Nature scientific journal, shed light on a promising pathway for awakening insulin-producing cells in individuals with type 1 diabetes.
The researchers, led by Professor Sam El-Osta, achieved a remarkable feat by demonstrating that newly generated insulin cells can respond to glucose and produce insulin within just 48 hours of stimulation using two FDA-approved drugs.
This discovery holds enormous potential for individuals ranging from the tender age of 7 to the mature age of 61, offering crucial insights into the mechanisms underlying the regeneration of beta cells.
Related Stories:
To conduct their groundbreaking experiments, the team utilized pancreatic cells obtained from both child and adult donors with type 1 diabetes, as well as cells from non-diabetic individuals.
They meticulously showcased how insulin-producing cells, which are typically destroyed in people with type 1 diabetes, can be regenerated into functional insulin-secreting cells with the ability to sense glucose levels.
One of the most noteworthy aspects of this research is the utilization of small molecule inhibitors, currently employed for rare cancers and sanctioned by the US FDA. These inhibitors were found to rapidly restore insulin production in pancreatic cells damaged by diabetes. Unlike current pharmaceutical treatments for diabetes that merely control blood glucose levels, this novel therapeutic approach offers the potential to become the first disease-modifying treatment for type 1 diabetes.
Researchers say the breakthrough could lead to an alternative treatment to regular insulin injections. (CREDIT: ABC Tropical North: Sophie Meixner)
Professor El-Osta expressed his optimism about this groundbreaking approach, stating, "We consider this regenerative approach an important advance towards clinical development." He emphasized that until now, the regenerative process had been largely incidental, lacking confirmation and a deep understanding of the epigenetic mechanisms governing such regeneration in humans.
The findings suggest that a mere 48 hours of stimulation with these small molecule inhibitors is sufficient to kickstart the process of insulin production from damaged pancreatic cells. Dr. Keith Al-Hasani, a JDRF Senior Research Fellow, highlighted that the next phase of their research involves investigating this regenerative approach in preclinical models.
The ultimate goal is to develop these inhibitors into pharmaceutical drugs that can restore insulin production in individuals living with diabetes.
The potential implications of this research are monumental. Not only does it hold promise for individuals with type 1 diabetes, but it also presents a hopeful solution for the significant portion of Australians living with insulin-dependent diabetes, constituting 30 percent of those with type 2 diabetes. Furthermore, it addresses the critical issue of donor organ shortages, providing an alternative avenue for treating diabetes without relying on organ transplants.
Pharmacological inhibition of EZH2 catalyses pancreatic progenitor activation and β-cell maturation. The schematic outlines the progression from pancreatic multipotent progenitors to mature insulin-secreting β-cells, highlighting the regulatory target of EZH2 inhibitors, GSK126 and Tazemetostat. (CREDIT: Nature)
As the world grapples with the rising diabetes epidemic, these findings offer a glimmer of hope. With more than 530 million adults currently living with diabetes, a number expected to surge to 643 million by 2030, the urgency to translate this research into tangible treatments cannot be overstated.
The potential to reduce the burden of round-the-clock insulin injections and revolutionize diabetes care is now closer than ever, thanks to the relentless pursuit of scientific discovery in the quest for a cure.
Note: Materials provided by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joshua Shavit
Science & Technology Writer | AI and Robotics Reporter
Joshua Shavit is a Los Angeles-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a contributor to The Brighter Side of News, he focuses on positive and transformative advancements in AI, technology, physics, engineering, robotics and space science. Joshua is currently working towards a Bachelor of Science in Business Administration at the University of California, Berkeley. He combines his academic background with a talent for storytelling, making complex scientific discoveries engaging and accessible. His work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.
