Bee-stinger microneedle patch speeds wound healing with smart monitoring
New bee-inspired microneedle patch speeds diabetic wound healing with insulin delivery, electrical therapy, and real-time monitoring.

Inspired by honeybees, scientists have built a microneedle patch that delivers insulin, stimulates healing, and tracks recovery in real time. (CREDIT: AI generated image / The Brighter Side of News)
Chronic wounds, especially those linked to diabetes, have long been one of the most frustrating challenges in medicine. Traditional bandages and ointments may help protect an injury, but they don’t do much to speed up recovery, control blood sugar, or track healing progress. Now, scientists in China say they’ve designed a device that can do all of that at once—thanks to a patch covered in tiny, bee-stinger-inspired needles.
Researchers at Shaanxi University of Science and Technology have developed a new microneedle patch that not only anchors securely under the skin but also delivers medication, stimulates tissue growth, and monitors recovery in real time. Their findings, published in the International Journal of Extreme Manufacturing, could mark a turning point in how doctors treat stubborn diabetic wounds.
A Bee-Inspired Design
The design takes its cues from honeybees. When a bee stings, its serrated stinger locks into the skin, preventing it from slipping out. The microneedles work in a similar way. Each has saw-toothed edges that grip the dermal layer of skin, keeping the patch stable even as a patient moves around during daily activities.
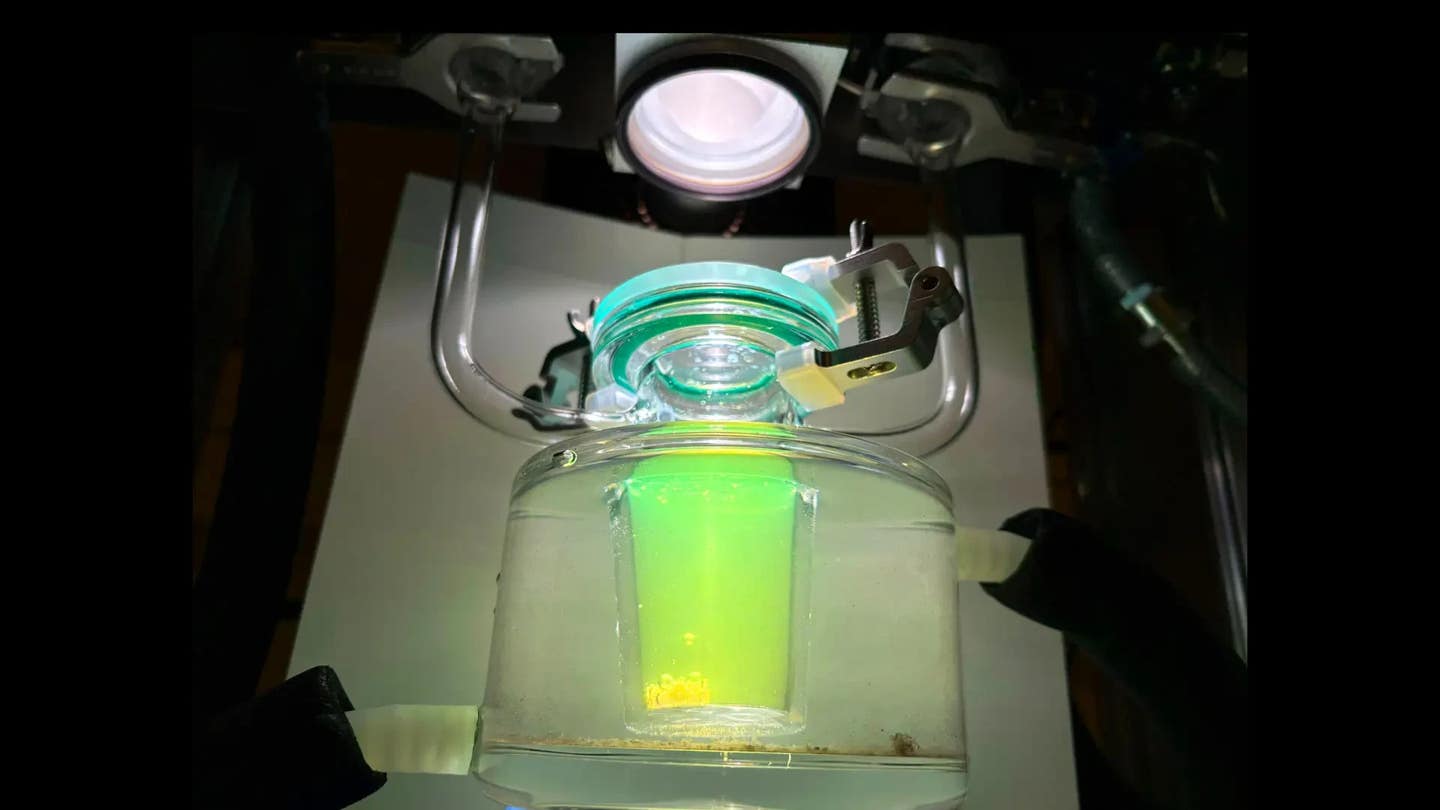
At the tip of every needle is a hydrogel that responds to body temperature. Once inserted, it steadily releases insulin for up to 24 hours, helping to stabilize blood sugar—one of the biggest hurdles to wound recovery in people with diabetes. At the same time, the base of the needles delivers mild electrical pulses. These signals encourage new blood vessel growth and stimulate surrounding tissue, while also measuring subtle changes in the wound’s electrical resistance, which serves as a marker of healing progress.
“This is more than a dressing,” said corresponding author Prof. Xinhua Liu. “It’s a real-time navigator for wound healing—a step toward truly personalized, data-driven care.”
Why Chronic Wounds Are So Hard to Treat
For people with diabetes, cuts and ulcers are more than just minor injuries. High blood sugar levels disrupt normal healing by weakening the immune system and reducing blood flow. Inflammation and bacterial infections often take hold, creating a damaging cycle that standard treatments can rarely break.
Related Stories
- 3D-printed heart patch made of living cells regrows damaged muscle
- Smart bandage tracks and treats chronic wounds in real time
Conventional approaches—gauze dressings, hydrogels, and ointments—may soothe discomfort and protect wounds from dirt, but they have clear limitations. They can’t actively lower glucose levels, provide deep antimicrobial action, or give doctors continuous updates about the wound’s status. As Prof. Liu explained, “Chronic wound management has long been a blind process. Clinicians often rely on visual checks, which means they can miss the critical moment for intervention.”
The microneedle system aims to change that. By combining drug delivery, electrical stimulation, and sensing in one patch, it turns wound care into an active, guided process rather than a passive waiting game.
Building the Patch
The team created the platform using biodegradable polylactic acid microneedles coated with polypyrrole, a conductive polymer. This coating allows electrical signals to move efficiently through the skin. At the tip, they attached a thermo-sensitive hydrogel made from amidated gelatin mixed with a smart polymer called PNIPAm. This material holds insulin until it reaches body temperature, then slowly releases the drug into the tissue.
The serrated needle structure gives the device the strength it needs to stay in place over time, while also reducing the risk of the needles bending or slipping out. Once secured, the patch performs a steady cycle of therapy: release insulin, stimulate tissue, and send data back through tiny sensors.
In laboratory and animal studies, the patch showed promising results. Wounds treated with the microneedle system healed 20 percent faster after 14 days compared to wounds treated with conventional methods. The steady release of insulin helped control blood sugar, while the electrical stimulation reduced infection risk and encouraged new blood vessel formation.
The device also demonstrated strong biocompatibility, meaning it worked smoothly with living tissue without causing harmful side effects. It successfully monitored changes in temperature and humidity at the wound site, giving researchers a real-time map of how healing was progressing.
Toward Smarter Healing and Personalized Care
The team isn’t stopping with this first version. They are working to add new sensing features, such as detecting biochemical markers that reveal infection or tissue damage earlier than visual signs. They also plan to develop artificial intelligence tools that could analyze wound data and automatically adjust the patch’s therapy—for example, increasing insulin release or changing the intensity of electrical stimulation when needed.
Another focus is comfort and wearability. For patients with diabetic foot ulcers, the device must withstand walking, exercise, and daily routines without causing irritation. Early prototypes show the rivet-like anchoring system is strong enough to hold steady while remaining comfortable, but researchers are refining the design to make long-term use even more practical.
Diabetes is one of the fastest-growing chronic illnesses in the world. Non-healing wounds lead to serious complications, including infections that sometimes require amputation. Innovations like this microneedle patch could reduce those risks and give patients more control over their own care.
By tracking healing progress minute by minute, the patch could allow doctors to make quicker decisions and prevent worsening conditions before they become dangerous. “We wanted to create a system that could see, decide, and act without removing the dressing,” Liu said. If future trials prove successful, this technology might transform how wound care is delivered, moving away from reactive treatment toward continuous, proactive therapy.
Past Studies and Findings
Microneedle-based drug delivery has been an area of intense study in recent years. Conventional solid microneedles offer strength but limited drug-carrying capacity, while dissolvable ones can deliver larger molecules but often lack durability. To address these issues, researchers have experimented with hybrid designs. Two-stage microneedles, for example, can deliver a drug-loaded tip into tissue while leaving a stable base behind. However, these systems still often fall out or fail to provide long-term therapy.
Other groups have explored adding electronic features. For instance, Lou et al. developed a flexible wound-healing patch that monitored temperature and alerted doctors to infections. Li et al. designed a microneedle electrode array that continuously measured biomarkers in diabetic patients. Qian et al. built a self-powered electronic microneedle that used triboelectric nanogenerator technology to deliver drugs and speed tissue repair in inflammatory skin diseases.
While each of these devices advanced the field, most faced limitations in controlled drug release, durability, or comprehensive sensing. The new bee-stinger-inspired patch integrates these elements into a single system, representing a significant step forward.
Practical Implications of the Research
If this technology moves successfully from lab to clinic, it could change everyday life for millions of people living with diabetes. A patch that actively manages blood sugar, fights infections, and tracks healing could reduce hospital visits, cut medical costs, and prevent amputations caused by untreated ulcers.
It could also pave the way for broader uses. Similar systems might one day be adapted for cancer therapy, post-surgery recovery, or even drug delivery for neurological conditions, where precise dosing and tissue monitoring are critical. By uniting bioelectronics with smart materials, researchers are opening the door to a new era of wearable, personalized medicine.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.