Breakthrough smartphone technology can help diagnose schizophrenia
Researchers shed light on the potential of leveraging smartphone sensing technology to devise standardized assessments for NSS.

[Sept. 16, 2023: Staff Writer, The Brighter Side of News]
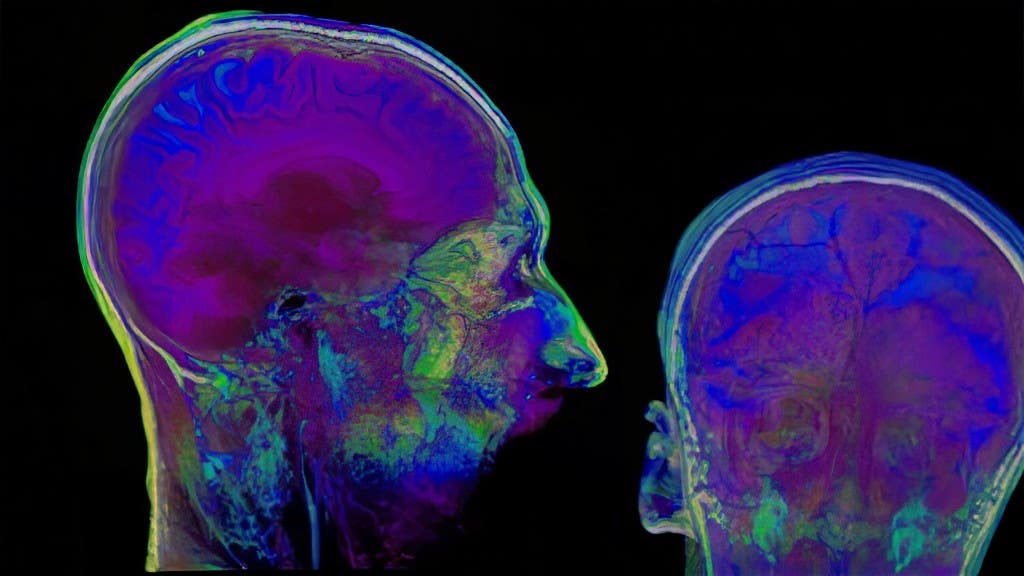
Religiosity and spirituality could be mapped to specific brain circuits. (CREDIT: Getty Images)
Objective measurement could improve patient management and aid research into how distinct groups of signs might reflect different aspects of psychiatric illness and neurologic impairment.
In a society fueled by technological innovations, the medical world often finds itself juxtaposed between traditional methods and new-age advancements. One such domain that has long been the focus of research and debate is the study of neurological soft signs (NSS) associated with schizophrenia.
Understanding Neurological Soft Signs (NSS)
First identified in the 1980s, NSS can distinguish individuals with schizophrenia from those without any psychiatric disorders. They are subtle neurological impairments that predominantly surface as:
Decreased Sensory Integration: Patients face difficulty in receiving and responding to information that is transmitted to their brain through the senses.
Balance Issues: Manifesting as vertigo or unsteadiness.
Challenges with Rapid Successive Movements: This could include tasks as simple as alternating hand movements.
Right-Left Orientation Difficulties: Impairments in distinguishing or using right and left directions.
While NSS doesn't always interfere with daily activities, pinpointing these signs can elevate the precision in diagnosing and treating schizophrenia. Furthermore, they provide a deeper comprehension of the disease's intricate nature.
However, challenges in assessing NSS have remained largely unaddressed for over four decades. The primary hurdle is the subjective nature of the rating systems for NSS, making it strenuous to consistently measure and compare deficits.
The Intersection of Technology and Medicine: A New Hope
Recently, in an enlightening article featured in the Harvard Review of Psychiatry— a commendable segment of the Lippincott portfolio from Wolters Kluwer—Dr. John Torous, MD, MBI, along with his adept team from Harvard's Beth Israel Deaconess Medical Center and the Massachusetts Mental Health Center in Boston, unveiled a groundbreaking perspective. They shed light on the potential of leveraging smartphone sensing technology to devise standardized assessments for NSS.
Related Stories
"In 2016, we introduced the term 'digital phenotyping,'" Dr. Torous explains. This refers to the novel use of data extracted from smart devices to discern behavior patterns capable of detecting illnesses.
In the realm of NSS, the sophisticated motion sensors embedded in our ubiquitous smartphones— like those that seamlessly toggle the display orientation or respond to intuitive gaming gestures— can unveil behavior patterns, potentially serving as NSS indicators.
To put this in perspective:
Balance Assessment: Envision a test where patients stand, their arms poised parallel to the ground, eyes shut for a minute. This could be replicated with a smartphone meticulously affixed to their chest, capturing every nuance of their balance.
Motor Coordination Examination: Drawing a parallel with Parkinson's disease assessment, patients could walk heel-to-toe in a regimented 12-foot line, all while a smartphone nestles in their pockets, documenting their every move.
Complex Motor Acts Test: Dive into the realm of sounds. A patient could mimic a sequence of auditory taps, guided and tracked by the rhythmic beats from a smartphone.
The implications of such intertwined tech-medical methodologies are profound. For starters, a smartphone can offer objective measurements, thereby enabling a quantitative evaluation of a patient's performance. This eradicates the examiner's subjective judgment of whether a patient exhibits impairments. Plus, embracing smartphones for NSS diagnostics can considerably abbreviate neurological consultations.
"Incorporating digital phenotyping into NSS assessment paves the way for a more scalable, accessible, and universally comparable measurement across diverse locations, cultures, and demographics," articulates Dr. Torous and his dedicated team. While certain tests might entail camera usage, contemporary security and data privacy measures can ensure data sanctity.
A World Transformed: The Nexus of Pandemic and Technology
One cannot discuss recent global events without referencing the profound impact of the COVID-19 pandemic, especially on the adoption of telehealth solutions. The pandemic catalyzed the swift uptake of remote health measures, amplifying patient confidence and intensifying privacy considerations.
Dr. John Torous, MD. (CREDIT: Creative Commons)
"This unprecedented era has crafted the perfect milieu to introduce and seamlessly integrate smartphone sensing technology and tools in NSS evaluation," the authors profoundly conclude.
In essence, as the world stands on the brink of numerous technological revolutions, the convergence of smartphones and medical diagnostics, particularly in the domain of schizophrenia and NSS, promises not only improved patient outcomes but a brighter, more informed future for the entire medical community.
For more science stories check out our New Discoveries section at The Brighter Side of News.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.