Breakthrough study challenges previous theories about Alzheimer’s disease
A new study challenges existing ideas of how buildup of a protein called amyloid beta (Aβ) in the brain is related to Alzheimer’s disease.
[Feb. 8, 2023: Orli Belman, USC Leonard Davis School of Gerontology]
A new study challenges existing ideas of how buildup of a protein called amyloid beta (Aβ) in the brain is related to Alzheimer’s disease. (CREDIT: Creative Commons)
A new USC Leonard Davis School of Gerontology study challenges existing ideas of how buildup of a protein called amyloid beta (Aβ) in the brain is related to Alzheimer’s disease.
While buildup of amyloid protein has been associated with Alzheimer’s-related neurodegeneration, little is known about how the protein relates to normal brain aging, said University Professor Caleb Finch, the study’s senior author and holder of the ARCO/William F. Kieschnick Chair in the Neurobiology of Aging at the USC Leonard Davis School.
To explore the levels of Aβ in human brains, the researchers analyzed tissue samples from both healthy brains and brains of patients with dementia. More severe Alzheimer’s cases were indicated by higher Braak staging scores, a measurement of how widely signs of Alzheimer’s pathology are found within the brain.
The analysis revealed that older, cognitively healthy brains showed similar amounts of dissolvable, non-fibrillar amyloid protein as brains of Alzheimer’s patients. But, as the researchers expected, the brains of Alzheimer’s patients had higher amounts of insoluble Aβ fibrils, the form of amyloid protein that aggregates to form the telltale “plaques” seen in the disease, said Max Thorwald, the study’s first author and a postdoctoral researcher at the USC Leonard Davis School.
Related Stories
The findings challenge the idea that simply having higher amounts of amyloid protein in general is an underlying cause of Alzheimer’s, say Finch and Thorwald. Instead, the increase in soluble Aβ may be a general aging-related change in the brain not specific to Alzheimer’s, while higher levels of fibrillary amyloid appear to be a better indicator of poorer brain health.
Rather than Alzheimer’s simply involving increased production of Aβ protein, the more important issue may be a reduced ability to effectively clear the protein and stave off the creation of plaque-contributing fibrillary amyloid, Thorwald said.
“These findings further support the use of aggregated, or fibrillary, amyloid as a biomarker for Alzheimer’s treatments,” Thorwald said. “The site in which amyloid processing occurs has less precursor and enzyme available for processing, which may suggest the removal of amyloid as a key issue during Alzheimer’s.”
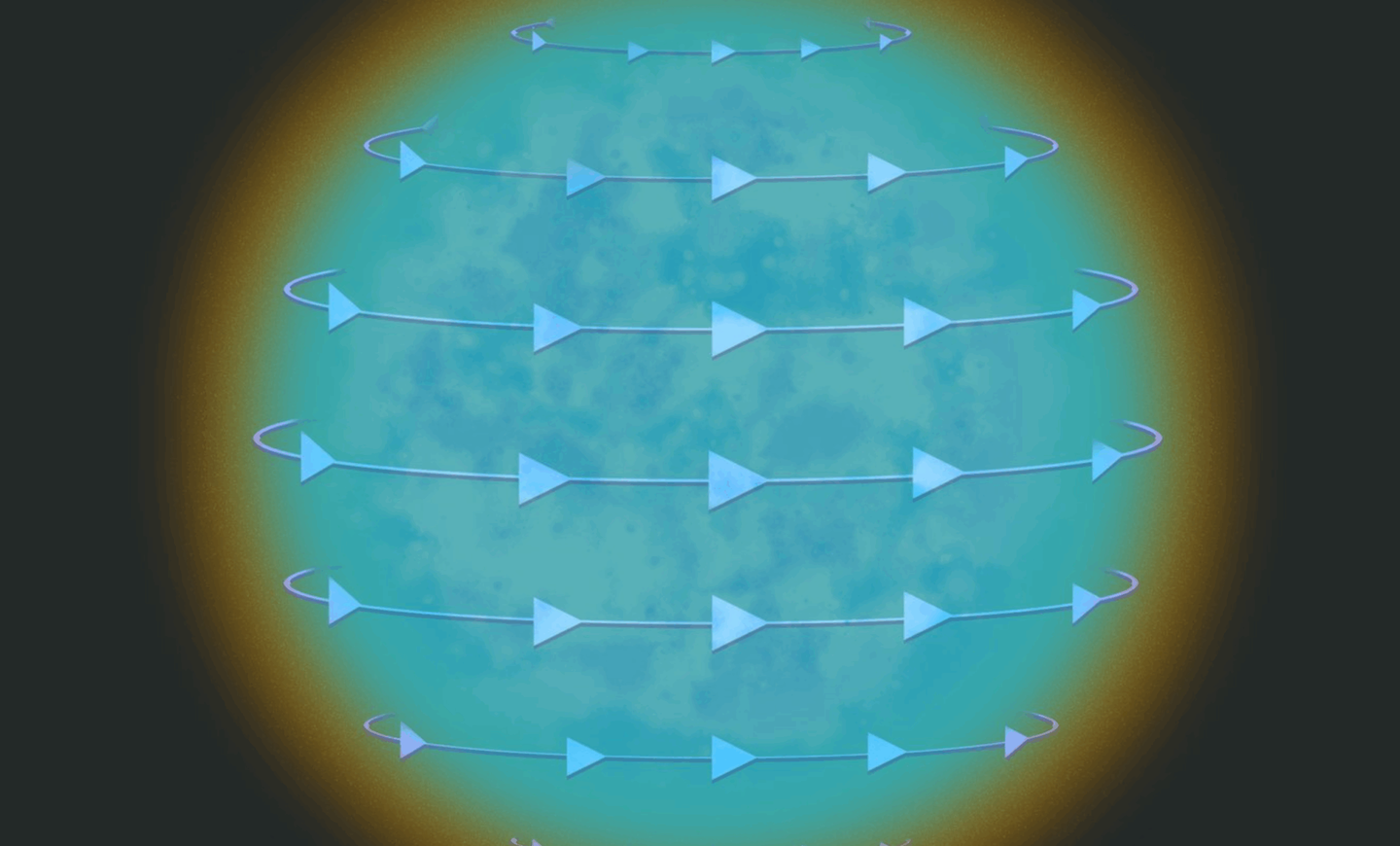
Correlation matrices examining relationships between soluble amyloid, lipid raft, and amyloid clearance for frontal cortex. (CREDIT: Alzheimer’s Association)
Increases in amyloid levels happen during early adulthood and differ by brain region. Further studies, including those investigating drugs to possibly break down amyloid, should incorporate positron emission tomography (PET) imaging in both healthy individuals and Alzheimer’s patients of a wide range of ages to determine how and where amyloid processing and removal changes in the brain over time, he added.
“The brain’s frontal cortex has more amyloid production compared to the cerebellum during the aging process in human brains, which coincides with their Alzheimer’s-correlated pathologies in late life,” Thorwald said. “Future projects should examine amyloid over the life course in both cognitively normal and Alzheimer’s patients with both modulation of amyloid processing or removal of amyloid through monoclonal antibodies currently used in clinical trials for Alzheimer’s treatment.”
Validation of lipid rafts (LRs). (A) Representative comparison of isolated human LRs from cognitively normal and Alzheimer's disease frontal cortex and cerebellum. (CREDIT: Alzheimer’s Association)
Monoclonal antibody treatment lemanecab has been observed to reduce Aβ plaques in clinical trials and recently received FDA approval for its potential to slow cognitive decline in Alzheimer’s patients, but the results warrant further careful research regarding long-term impact, Finch said.
"Lecanemab clearly works to diminish fibrillar amyloid," he said. "However, we are concerned with major side effects, including brain swelling and bleeding, that were 100% more than in controls, with unknown delayed or latent impact."
Correlation matrices examining relationships between soluble amyloid, lipid raft, and amyloid clearance for frontal cortex and cerebellum. (CREDIT: Alzheimer’s Association)
Learning more about how the brain processes and removes proteins such as Aβ could provide important insights into Alzheimer’s disease and its causes.
Finch noted that very few cases of dementia occur with amyloid plaques, or masses of aggregated Aβ protein, as the only pathology present in affected patients’ brains. Instead, most cases present with more complicated tissue abnormalities, from buildup of additional types of protein to small bleeds in the brain: “The aging brain is a jungle.”
Note: Materials provided above by USC Leonard Davis School of Gerontology. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.