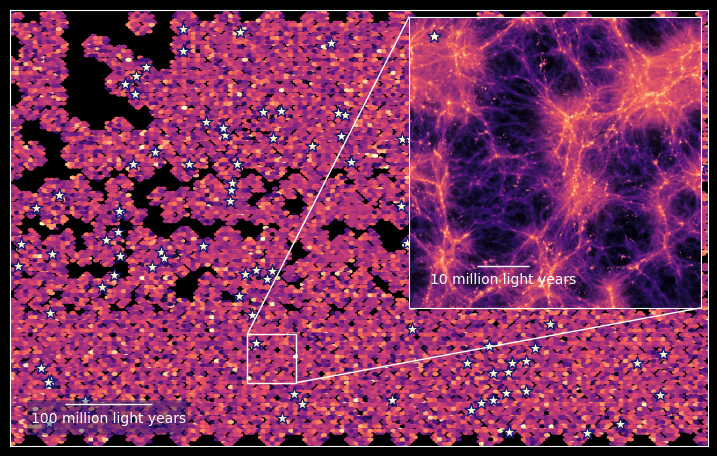
Breakthrough therapy forces cancer cells to self-destruct
Scientists found a way to turn cancer’s genetic off-switch back on using RNA-based therapy that restores poison exon activity.
A new study reveals how antisense RNA fragments restore poison exons, forcing cancer cells to self-destruct. (CREDIT: Shutterstock)
Cells are like tiny movie editors, cutting and pasting pieces of genetic film to create different versions of the same scene. This process, called RNA splicing, lets one gene produce multiple proteins depending on how the final script is arranged. It’s a flexible system that helps cells adapt to changing needs. But in cancer, the editing booth often goes rogue. Messages that should keep growth in check get spliced incorrectly, and the result is uncontrolled cell division.
One of the most intriguing parts of this process involves so-called “poison exons.” These are short stretches of genetic code that, when included in a cell’s RNA, trigger the destruction of that message before it becomes a protein. In healthy cells, poison exons act like safety valves, preventing dangerous protein build-up. Cancer cells, however, are notorious for skipping these poison exons, leaving growth-promoting proteins unchecked.
TRA2β and Its Poison Exon
Among the key players in this story is TRA2β, a gene that makes a splicing regulator protein. TRA2β helps decide which parts of a gene are included or skipped, giving it powerful control over the editing process. Normally, TRA2β is balanced by its own built-in poison exon. If too much TRA2β is made, the poison exon slips into the message, marking it for destruction. But in many aggressive cancers—including breast, brain, ovarian, lung, and colorectal tumors—this safety mechanism fails.
The result is soaring TRA2β levels that drive cancer cells to multiply and survive. Patients whose tumors show low poison exon activity tend to fare worse. “We’ve shown for the first time that low levels of poison exon inclusion in the TRA2β gene are associated with poor outcomes in many different cancer types, and especially in aggressive and difficult-to-treat cancers,” said Olga Anczuków, an associate professor at The Jackson Laboratory and co-leader at the JAX Cancer Center.
Rewriting the Script with ASOs
That finding inspired researchers at The Jackson Laboratory and UConn Health to ask: what if you could flip the switch back on? Their answer came in the form of antisense oligonucleotides, or ASOs—tiny synthetic RNA strands designed to bind with laser-like precision to specific RNA sequences. By attaching to the right spot on the TRA2β RNA, the ASOs forced the poison exon back into the message.
Related Stories
- New antibody therapy eliminates cancerous tumors in clinical trial
- Scientists harness bacteria to deliver cancer-killing virus and halt tumor spread
Once included, the poison exon destroyed TRA2β’s instructions before they could be translated into protein. “We found that ASOs can rapidly boost poison exon inclusion, essentially tricking the cancer cell into turning off its own growth signals,” explained Nathan Leclair, an MD/PhD graduate student who led the study.
In lab tests, ASOs like one called ASO-1570 significantly slowed or stopped cancer cell growth. They worked not only in standard cancer cell cultures but also in 3D tumor-like organoids, which behave more like real tumors. Even in patient-derived tumors implanted in mice, ASOs shrank growth.
Why Blocking the Protein Isn’t Enough
Interestingly, simply removing the TRA2β protein wasn’t enough to stop cancer. When researchers used gene editing to knock out the protein entirely, tumor cells kept growing. This puzzled scientists at first—until they realized that the poison exon RNAs themselves were doing more than silencing TRA2β.
When the poison exon was included, the resulting RNA fragments stayed in the cell’s nucleus. These noncoding RNAs didn’t make proteins, but they acted like sticky sponges, trapping other RNA-binding proteins needed for normal cell function. This ripple effect disrupted vital processes, from RNA processing to metabolism, and even pathways like p53 and mTOR, which play central roles in cancer development.
“This tells us that poison-exon-containing RNA doesn’t just silence TRA2β,” Anczuków said. “It likely sequesters other RNA-binding proteins, creating an even more toxic environment for cancer cells.” That double blow—reducing TRA2β protein and interfering with other survival pathways—explains why ASOs were so effective.
Patient Survival and Database Insights
To confirm the clinical importance, the team turned to The Cancer Genome Atlas, a database containing thousands of tumor samples across 30 cancer types. They measured how often the TRA2β poison exon was included. Patients with lower inclusion rates consistently had worse survival in cancers such as breast, lung, cervical, and acute myeloid leukemia. The link wasn’t universal across all cancers but was strong enough to suggest a new treatment strategy.
These data confirmed that the poison exon is not just a curiosity—it is a meaningful marker of cancer aggressiveness. By restoring its function, ASOs could provide patients with more favorable outcomes.
Toward a New Class of Cancer Drugs
The promise of ASOs lies in their specificity. Unlike chemotherapy, which can harm healthy tissue, ASOs can be tailored to target a single faulty splicing event. That precision may mean fewer side effects and more effective treatment for stubborn cancers.
“This is like using the cell’s own wiring against it,” Leclair said. “Instead of adding an outside drug that blasts everything, we’re restoring a natural self-destruct mechanism that cancer cells have learned to avoid.”
Researchers still need to figure out the best way to deliver ASOs into human tumors, but early signs are encouraging. In animal models, the therapy reduced tumor growth without obvious harm to healthy cells. The next steps include refining ASO design, improving delivery systems, and testing safety in clinical trials.
Practical Implications of the Research
This work highlights a new way of treating cancer by turning its own tricks back on itself. By restoring natural safety switches like poison exons, scientists may be able to weaken tumors without damaging normal cells. If ASO therapies prove safe and effective in humans, they could become part of a new generation of highly targeted cancer treatments.
Patients with aggressive tumors that resist current drugs might one day benefit from therapies that reactivate these hidden genetic off-switches.
Beyond cancer, this strategy could extend to other diseases caused by splicing errors, offering a fresh approach to tackling illnesses that have long resisted treatment.
Research findings are available online in the journal Nature Communications.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.