Common cold can give children immunity against COVID-19, study finds
During the pandemic medical doctors and researchers noticed that children and adolescents infected with COVID-19 became less ill than adults

[Mar. 19, 2023: Felicia Lindberg, Karolinska Institutet]
Scientists have discovered a protein in the lung that blocks SARS-CoV-2 infection and forms a natural protective barrier in the human body.(CREDIT: Creative Commons)
During the pandemic, medical doctors and researchers noticed that children and adolescents infected with COVID-19 became less ill than adults. A possible explanation for this is that children already had a prior level of immunity to COVID-19 provided by memory T cells generated by common colds.
After studying unique blood samples from children taken before the pandemic, researchers from Karolinska Institutet in Sweden have now identified memory T cells that react to cells infected with SARS-CoV-2, the virus that causes COVID-19.
Four coronaviruses cause common colds
A possible explanation for this immunity in children is that they already had colds caused by one of the four coronaviruses causing seasonal common cold symptoms. This could stimulate an immune response with T cells able to also react to cells infected with SARS-CoV-2.
This new study reinforces this hypothesis and shows that T cells previously activated by the OC43 virus can cross-react against SARS-CoV-2.
Related Stories:
“These reactions are especially strong early in life and grow much weaker as we get older,” says the study’s corresponding author Annika Karlsson, research group leader at the Department of Laboratory Medicine, Karolinska Institutet.
“Our findings show how the T-cell response develops and changes over time and can guide the future monitoring and development of vaccines.”
Strong immunity at the age of two
The results indicate that the memory T-cell response to coronaviruses develops as early as the age of two. The study was based on 48 blood samples from two- and six-year-old children, and 94 samples from adults between the ages of 26 and 83. The analysis also included blood samples from 58 people who had recently recovered from COVID-19.
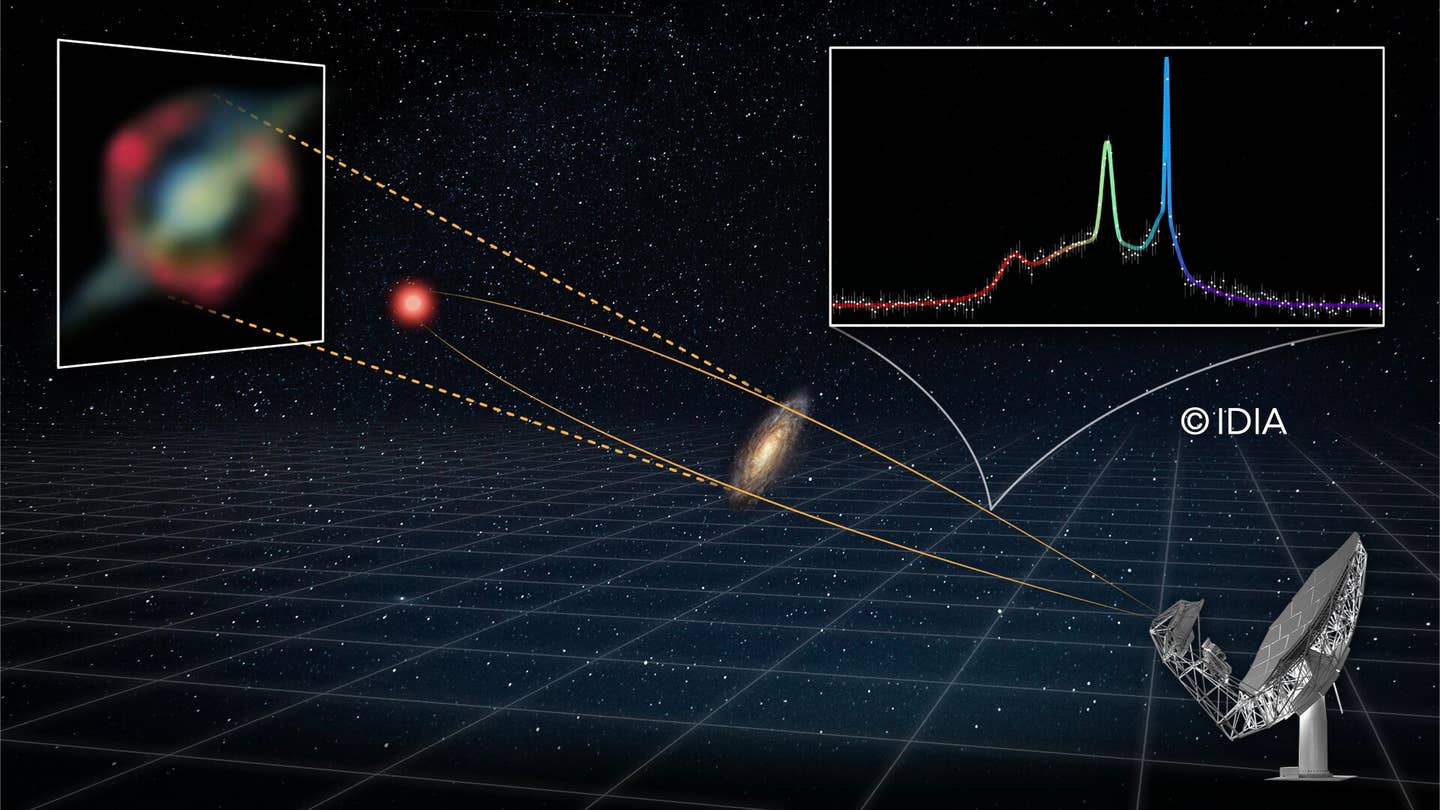
Study outline and mapping of T cell responses against OC43 and SARS-CoV-2. (CREDIT: Proceedings of the National Academy of Sciences)
“Next, we’d like to do analogous studies of younger and older children, teenagers and young adults to better track how the immune response to coronaviruses develops from childhood to adulthood,” says Marion Humbert, postdoctoral researcher currently at the Department of Medicine Huddinge, Karolinska Institutet, joint first author with Anna Olofsson, doctoral student at the Department of Laboratory Medicine.
How likely is it for a child to become sick with coronavirus disease 2019 (COVID-19)?
According to the Mayo Clinic, children represent about 19% of all reported COVID-19 cases in the U.S. since the pandemic began.
While children are as likely to get COVID-19 as adults, kids are less likely to become severely ill. Up to 50% of children and adolescents might have COVID-19 with no symptoms. However, some children with COVID-19 need to be hospitalized, treated in the intensive care unit or placed on a ventilator to help them breathe.
Certain medical conditions might increase a child's risk of serious illness with COVID-19, including:
Obesity
Diabetes
Asthma
Congenital heart disease
Genetic conditions
Conditions affecting the nervous system or metabolism
Research also suggests disproportionately higher rates of COVID-19 in Hispanic and non-Hispanic Black children than in non-Hispanic white children.
Can children who get COVID-19 experience long-term effects?
Again, according to the Mayo Clinic, anyone who has had COVID-19 can develop a post-COVID-19 condition. Research suggests that children with both mild and severe COVID-19 have experienced long-term symptoms. The most common symptoms in children include:
Tiredness or fatigue
Headache
Trouble sleeping
Trouble concentrating
Muscle and joint pain
Cough
These symptoms could affect your child's ability to attend school or do his or her usual activities. If your child is experiencing long-term symptoms, consider talking to your child's teachers about his or her needs.
The paper cited above is the result of a collaborative study among researchers at Karolinska Institutet, the universities of Bern (Switzerland), Oslo (Norway) and Linköping University (Sweden).
The study was financed by the Swedish Research Council, Region Stockholm (CIMED), Karolinska Institutet, the Knut and Alice Wallenberg Foundation and the European Research Council. Karl-Johan Malmberg, Ebba Sohlberg and Soo Aleman receive fees from companies and organisations outside this research project (see the paper for more details); all other researchers report no conflicts of interest.
Note: Materials provided above by Karolinska Institutet. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.