First-of-its-kind therapy revolutionizes chronic pain treatment
Chronic pain, a health issue plaguing approximately one-third of the U.S. population, has often found scientists at a odds for treatment

[Oct 7, 2023: Staff Writer, The Brighter Side of News]
Chronic pain is a health issue plaguing approximately one-third of the U.S. population. (CREDIT: Creative Commons)
Chronic pain, a health issue plaguing approximately one-third of the U.S. population, has often found scientists at a odds when it comes to formulating effective treatments.
However, the team at NYU College of Dentistry’s Pain Research Center, under the guidance of Rajesh Khanna, director of the NYU Pain Research Center and professor of molecular pathobiology, has taken a significant stride in gene therapy that holds the promise of treating chronic pain. Their pioneering research focuses on the intricate relationship between the NaV1.7 sodium ion channel and a regulatory protein.
Targeting the Sodium Ion Channel
The mechanism of pain perception in our body can be traced back to sodium ion channels which play a pivotal role in nerve cells or neurons communicating with each other. Within this context, the NaV1.7 sodium ion channel emerges as a focal point. Genetic mutations in this channel have been linked with extreme pain conditions, and as a result, it has been under the microscope for potential therapeutic interventions.
In particular, Rajesh Khanna has illuminated the key interaction between NaV1.7 and a protein named CRMP2. “CRMP2 ‘talks’ to the sodium ion channel and modulates its activity, allowing more or less sodium into the channel.
Related Stories
If you block the conversation between Nav1.7 and CRMP2 by inhibiting the interaction between the two, we can dial down how much sodium comes in. This quiets down the neuron and pain is mitigated,” explained Khanna in the recent study published in the Proceedings of the National Academy of Sciences (PNAS).
Rather than blocking NaV1.7 directly, which has seen limited success in the past, Khanna's team has decided to indirectly regulate it. Their research previously identified a compound that regulates Nav1.7 expression through targeting CRMP2.
This compound has shown promise in controlling pain in both cellular and animal models, marking an initial victory in the fight against chronic pain. However, a lingering question remained: Why does CRMP2 specifically communicate with the NaV1.7 sodium ion channel?
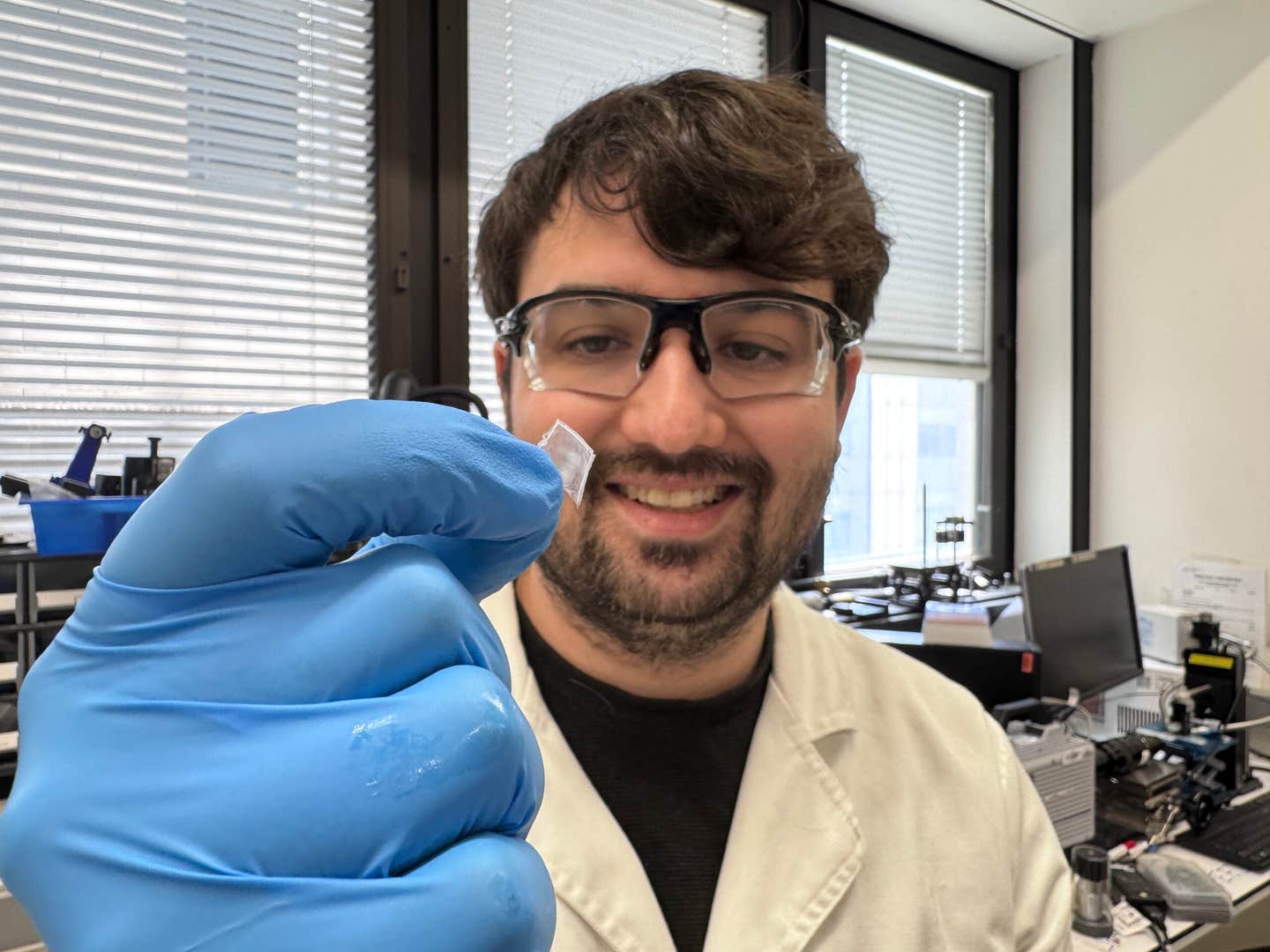
An artistic representation of the interaction between the NaV1.7 sodium ion channel and collapsin response mediator protein 2 (CRMP2). (CREDIT: Samantha Perez-Miller and Rajesh Khanna (New York University))
Through meticulous research, the team zeroed in on the unique region within NaV1.7 where CRMP2 binds. “This got us really excited, because if we took out that particular piece of the NaV1.7 channel, the regulation by CRMP2 was lost,” Khanna remarked.
Gene Therapy: A Beacon of Hope
Capitalizing on their discovery, the researchers used a peptide from the unique region in NaV1.7 where CRMP2 binds and inserted it into an adeno-associated virus. The intent was to inhibit NaV1.7. Using viruses in this manner – to carry genetic material into cells – is a pioneering approach in gene therapy. Previous successes include treatments for blood disorders, eye diseases, and other rare conditions.
Identification of a unique CRMP2 regulatory domain on NaV1.7. Cartoon of the domain structure of human NaV1.7 with intracellular loops labeled. These loops were divided into 384 15-mer peptides with 12 overlapping amino acids and were printed onto a peptide array. (CREDIT: PNAS)
The engineered virus was administered to mice exhibiting pain symptoms. Remarkably, in just a week to ten days, the pain these animals experienced had reversed.
“We found a way to take an engineered virus—containing a small piece of genetic material from a protein that all of us have—and infect neurons to effectively treat pain,” Khanna stated enthusiastically, adding, “We are at the precipice of a major moment in gene therapy, and this new application in chronic pain is only the latest example.”
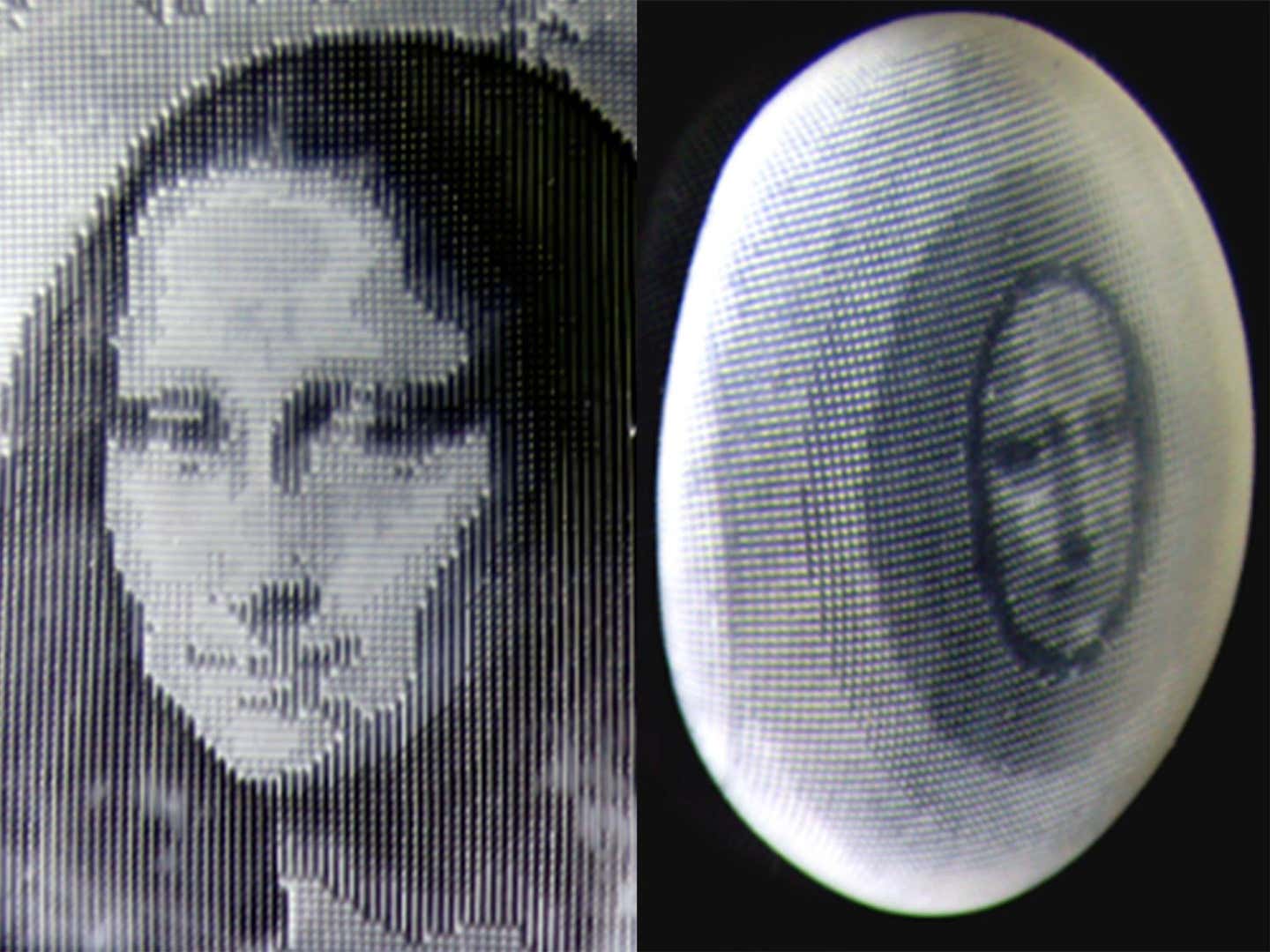
Myr-TAT-NaV1.7-CRS causes CRMP2 dependent reduction in NaV1.7 currents in DRG neurons. (A) The Myr-TAT-NaV1.7-CRS peptide competes for binding to NaV1.7 regulatory proteins. (CREDIT: PNAS)
This groundbreaking approach was also tested across various species, including rodents and cells from primates and humans. The results hint at a promising future, suggesting that such treatments might soon be applicable to humans.
The Road Ahead
While the initial results are promising, further studies are paramount. Khanna envisions a world where gene therapy could be used extensively to treat painful conditions, especially for patients undergoing chemotherapy.
Disruption of the NaV1.7-CRMP2 interaction decreases presynaptic NaV1.7, sensory neuron excitability, and spinal cord neurotransmitter release. (CREDIT: PNAS)
“There is a significant need for new pain treatments, including for cancer patients with chemotherapy-induced neuropathy. Our long-term goal is to develop a gene therapy that patients could receive to better treat these painful conditions and improve their quality of life,” Khanna emphasized.
As the world watches, the endeavor to combat chronic pain through gene therapy exemplifies the innovative spirit of modern science. Through meticulous research and a nuanced understanding of the intricacies of our body's pain mechanisms, scientists like Rajesh Khanna and his team are forging a path to a future where chronic pain might be a thing of the past.
Chemogenetics has shown promise as a means to suppress such excitability, yet chemogenetic approaches suitable for human applications are needed. PSAM4-GlyR is a modular system based on the human α7 nicotinic acetylcholine and glycine receptors, which responds to inert chemical ligands and the clinically approved drug varenicline. (CREDIT: Science)
Related gene therapy research at the University of Oxford
Researchers from the Nuffield Department of Clinical Neurosciences at the University of Oxford, along with colleagues at Cambridge University and Barts and the London School of Medicine and Dentistry, have shown the potential of a new gene therapy approach to silence human sensory neurons (nerve cells) as a means of treating persistent pain.
Chemogenetics is a process where molecules that control the excitation (stimulation) of neurons are engineered so they only become active in the presence of a non-toxic drug. This process has already shown promise as a means of suppressing such excitability in research involving animals. Jimena Perez-Sanchez, a postdoctoral research scientist at the Nuffield Department of Clinical Neurosciences and joint author of the study with Steven Middleton, and her colleagues have now shown that there is a chemogenetic approach that is suitable for human applications.
First, the team expressed the gene PSAM4-GlyR, a chemogenetic system based on the human protein receptors nicotinic acetylcholine and glycine, in mouse sensory neurons. They activated PSAM4-GlyR with the clinically approved drug varenicline, which inhibited sensory neurons and also reduced the pain hypersensitivity normally associated with arthritis or nerve injury in mice.
Then, the researchers went on to activate the PSAM4-GlyR system in sensory neurons derived from a patient with erythromelalgia, a condition characterised by burning pain. They found that this inhibited the neurons and normalised hyperactivity.
David Bennett, Professor of Neurology and Neurobiology and Jimena Perez-Sanchez, postdoctoral research scientist at the Nuffield Department of Clinical Neurosciences, commented: ‘The whole team are pleased to have shown the potential of a gene therapy approach for the treatment of chronic pain which remains one of the great unmet health needs. This has been achieved by switching off hyperactive nerve fibres. By targeting this initial component of the pain circuit we could avoid the addictive potential of existing pain killers such as opioids.’
Although further validation in human pain models is needed, the results demonstrate the contribution of sensory neuron hyperexcitability to persistent pain due to arthritis or injury to the nervous system. The researchers have shown the translational potential of engineering human protein receptors for the treatment of pain.
For more science and technology stories check out our New Innovations section at The Brighter Side of News.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.