Gamechanging antibody neutralizes all known variants of SARS-CoV-2
As the COVID-19 pandemic continues, emerging variants of SARS-CoV-2 have been developing methods to circumvent the antibodies we produce.
[Sept. 10, 2023: Staff Writer, The Brighter Side of News]
Scientists have been searching for an antibody that would be broadly neutralizing — able to fight off any viral variant that might emerge. (CREDIT: Creative Commons)
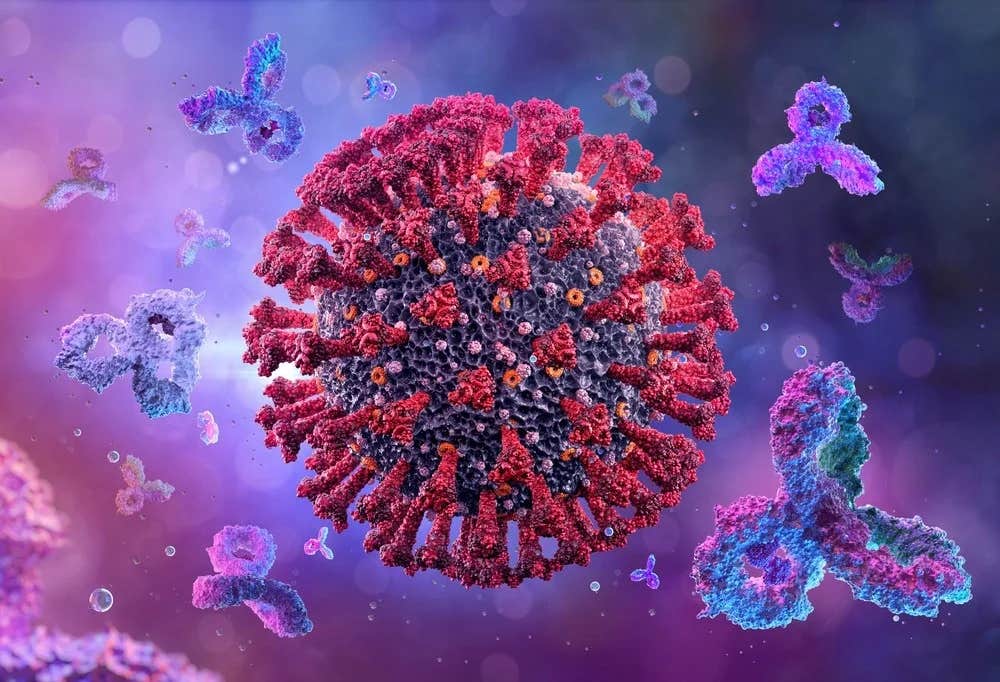
As the progression of the COVID-19 pandemic continues, emerging variants of SARS-CoV-2 have been developing methods to circumvent the antibodies produced by our immune systems in reaction to vaccination or previous infections. This has led to cases of breakthrough infections, and the diminishing efficacy of antibody treatments over time.
Researchers have been on a quest to identify a universally neutralizing antibody capable of combating any potential viral variant that could surface.
Researchers from Harvard Medical School and Boston Children's Hospital have made a significant breakthrough with the development of a new antibody.
This antibody, during laboratory examinations, effectively neutralized all presently recognized variants of SARS-CoV-2, which includes all known variants of Omicron.
Frederick Alt, the Charles A. Janeway Professor of Pediatrics at Boston Children's, Professor of Genetics at HMS, and a senior investigator of the study, expressed optimism, stating, "We hope this antibody will prove to be as effective in patients as it has been in preclinical evaluations thus far."
Related Stories:
“If it does,” he added, “it might provide a new therapeutic and also contribute to new vaccine strategies.”
Creating and testing multiple antibodies
Under the leadership of Alt and Sai Luo, a pediatrics instructor at Boston Children’s from HMS, the team initially altered a mouse model, originally developed by the Alt lab, to investigate broadly neutralizing antibodies against HIV, a virus known for its high mutation rate. Essentially, these mice possess human immune systems within them.
The revised model emulates and enhances the iterative process by which our immune systems generate increasingly potent antibodies when faced with a pathogen.
Initially, the scientists integrated two human gene segments into the mice. This action stimulated the rodents' immune cells to rapidly synthesize a broad array of antibodies, akin to the ones our bodies could potentially create.
Subsequently, the group exposed the mice to the SARS-CoV-2 spike protein, the primary protein that our antibodies and existing vaccines aim at, derived from the initial Wuhan-Hu-1 coronavirus variant.
As a reaction, the mice generated nine distinct groups of antibodies that attached themselves to the spike protein.
In partnership with colleagues at Duke University, Alt and Luo evaluated the potency of these generated antibodies.
Three out of the nine identified antibody families exhibited significant effectiveness in neutralizing the original Wuhan-Hu-1 virus. However, one particular antibody family, most notably the antibody designated as SP1-77, demonstrated a more extensive range of activity, neutralizing alpha, beta, gamma, delta, and all previously and currently known omicron strains.
A new way to neutralize
What characteristics make SP1-77 so efficient at neutralizing the virus? Through the combined efforts of structural biology studies conducted by teams led by Bing Chen, the Rosalind Franklin, PhD Professor of Pediatrics at Boston Children’s; Jun Zhang, HMS instructor in pediatrics at Boston Children’s; and Barton Haynes at Duke, it was discovered that this antibody functions in a distinct manner.
For SARS-CoV-2 to infect human beings, it must first bind to ACE2 receptors on our cells. Many of the antibodies produced in response to vaccines, as well as those used in the treatment of COVID-19, inhibit this binding process. They achieve this by attaching to the spike’s receptor-binding domain at specific sites.
The SP1-77 antibody, however, interacts with the receptor-binding domain in a unique way that does not stop the virus from binding to ACE2 receptors.
So how would it protect us?
After the virus attaches itself to ACE2, it has to perform a concluding process: integrating its exterior membrane with the membrane of our cells. This effectively paves the way for infection. With the help of a unique live-cell imaging platform, Alex Kreutzberger, an instructor in pediatrics at Boston Children’s from HMS, and Tomas Kirchhausen, a professor of cell biology at the Blavatnik Institute at HMS and also a professor of pediatrics at Boston Children’s, demonstrated that SP1-77 halts this process.
“SP1-77 binds the spike protein at a site that so far has not been mutated in any variant, and it neutralizes these variants by a novel mechanism,” noted Kirchhausen. “These properties may contribute to its broad and potent activity.”
Next steps
Should these discoveries be successfully duplicated in humans, these antibodies might pave the way for improved COVID-19 vaccines and therapies.
The scientists have submitted patent applications for both the antibodies and the mouse model employed in their generation. Their aspiration is to see their research evolve into commercial applications.
“It was a pleasure to work with this dedicated collaborative team whose diverse expertise allowed SP1-77 to be brought to light,” said Alt. “We look forward to using our models to discover antibodies with therapeutic potential against other newly emerging pathogens.”
This work was supported by the Howard Hughes Medical Institute, the Bill & Melinda Gates Foundation (INV-021989), the National institutes of Health (NIAID Consortia for HIV/AIDS Vaccine Development UM1-AI144371, P01 AI158571, Maximizing Investigators’ Research Award GM130386, Harvard Virology Program training grant T32 AI07245), Massachusetts Consortium on Pathogen Readiness (MassCPR) SARS-CoV-2 Variants Award, Emergent Ventures fast grant, FDA (MCMi grant #OCET 2021-1565 and Perinatal Health Center of Excellence project grant #GCBER005), the Danish Technical University and SANA, and IONIS.
Disclosures: Alt and study coauthor Ming Tian of HMS and Boston Children’s are authors on a patent application that describes the general type of mouse model used. Luo, Haynes, and Alt are authors on patent applications describing the antibodies reported.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.