Gamechanging gene editing tool dramatically improves cancer immunotherapy
Recent scientific advances have transformed immune cells into power-packed therapeutics trained to target malignancies.
[Sept. 18, 2023: Staff Writer, The Brighter Side of News]
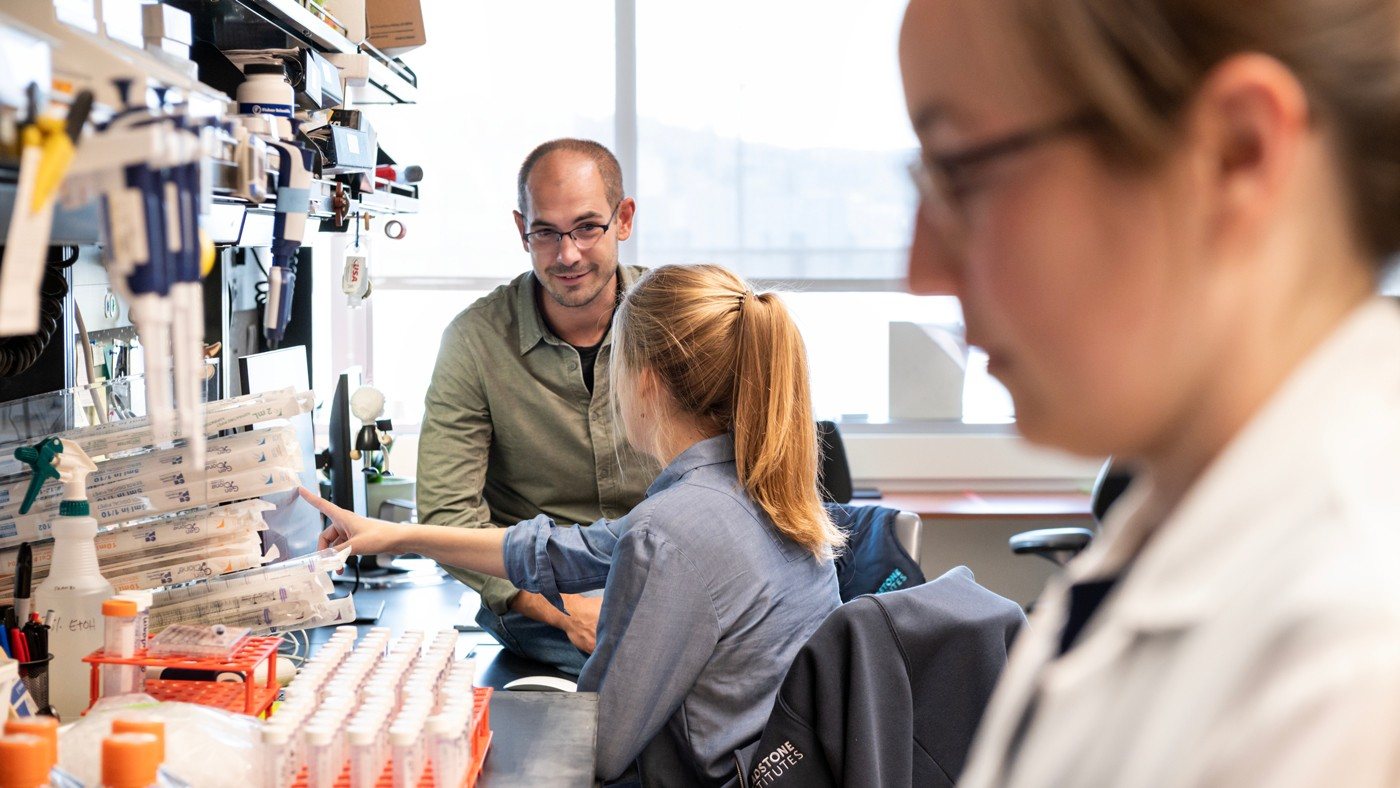
Researchers at Gladstone Institutes and UC San Francisco—including Theodore Roth (left) and Franziska Blaeschke (center)—used a new method to screen 10,000 combinations of gene edits in immune cells engineered to fight cancer. (CREDIT: Gladstone Institutes)
In the escalating battle against cancer, our immune cells have emerged as unlikely heroes. Recent scientific advances have transformed these cells into power-packed therapeutics trained to target malignancies. But like any hero, these cells have their kryptonite—limitations preventing them from universally conquering all cancer types.
However, a groundbreaking development from the Gladstone Institutes and UC San Francisco (UCSF) might soon change this narrative.
They've birthed a technology, named Modular Pooled Knockin Screening (ModPoKI), that can swiftly experiment with thousands of genetic edits, paving the way for enhanced reprogrammed immune cells to tackle cancer more efficiently.
Revolutionizing Genetic Programming
Over the years, we've witnessed the immense potential of immunotherapies. Yet, their scope remains limited. "This is a major step forward in our ability to ask questions about how we put pieces of genetic programs together into cells and test how they may be advantageous for patients,” notes Alex Marson, MD, PhD, director of the Gladstone-UCSF Institute of Genomic Immunology.
Related Stories
Ansuman Satpathy, MD, PhD, from Gladstone and Stanford School of Medicine, further emphasizes the importance of this study, stating, “This study demonstrates the power of using high-throughput genomics to discover and engineer novel molecular programs in cell therapies.”
Central to our body's defense mechanism are the T cells, constantly scouting for harmful foreign entities, including cancer cells. With their unique ability to identify and eliminate cancer cells, they are prime candidates for genetic modifications.
One such intervention is the insertion of a chimeric antigen receptor (CAR), enhancing the T cells' recognition capabilities. The modus operandi of CAR T-cell therapy is fascinating. T cells are harvested from a patient, genetically modified to house the new CAR receptors, and then reintroduced into the patient. But this isn’t a magic bullet.
Graphical abstract: ModPoKI facilitates the discovery of complex gene constructs to program cellular functions. (CREDIT: Cell Press)
"CAR T cells have been incredibly successful in the treatment of blood cancers like leukemia and lymphoma, but we’re still searching for ways to optimize them and apply them to other cancers,” observes Franziska Blaeschke, MD, PhD, from Marson’s lab.
ModPoKI: The Future of Genetic Screening
Filling the existing knowledge gap, ModPoKI emerges as a transformative tool. This technology ingeniously stitches together multiple genes, allowing them to be used in a CRISPR gene editing platform. The researchers have thus far tested approximately 10,000 DNA combinations using this technique.
Schematic illustration of the ModPoKI platform. Barcoded multicistronic adaptors allowed for modular cloning, barcode sequencing, and translation of separate proteins. A furin sequence was included to help remove 2A residues from the upstream gene product. (CREDIT: Gladstone Institutes)
The sheer innovation lies in its efficiency. Theodore Roth, MD, PhD, elucidates, “Rather than having to make individual guesses about what might improve the function of cells and work through them one by one, we can click these pieces together and very rapidly test many of them in succession.”
The Path to Enhanced Cellular Therapies
The team's latest endeavor involved infusing cells with both surface receptors (natural and engineered) and transcription factors. After analyzing results from these insertions, they found that different CARs required distinct optimizations. A significant takeaway was the identification of two transcription factors, BATF and TFAP4, which seemed to augment the capabilities of CAR T cells, specifically those designed for childhood brain tumors.
A group of researchers, including Roth (left) and Blaeschke (right), developed a screening technology called ModPoKI to stitch together and compare different DNA sequences in order to discover which ones might improve CAR T cells. (CREDIT: Gladstone Institutes)
“Next, we need to do more work to determine whether adding these transcription factors will make CAR T cells more effective in human cancer patients,” cautions Marson.
The journey of reimagining our immune cells to fight cancer is an ongoing one, fraught with challenges and excitement. Yet, with tools like ModPoKI, scientists are steadily edging closer to unlocking the full potential of our immune cells, heralding a new era in cancer therapeutics. For patients and healthcare professionals worldwide, the horizon looks promising, with the promise of a future where cancer can be tackled more effectively.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.