Groundbreaking topical gel relieves ear infections in just one dose
Scientists developed a single-dose antibiotic gel that cures middle ear infections safely, reducing side effects and antibiotic resistance.

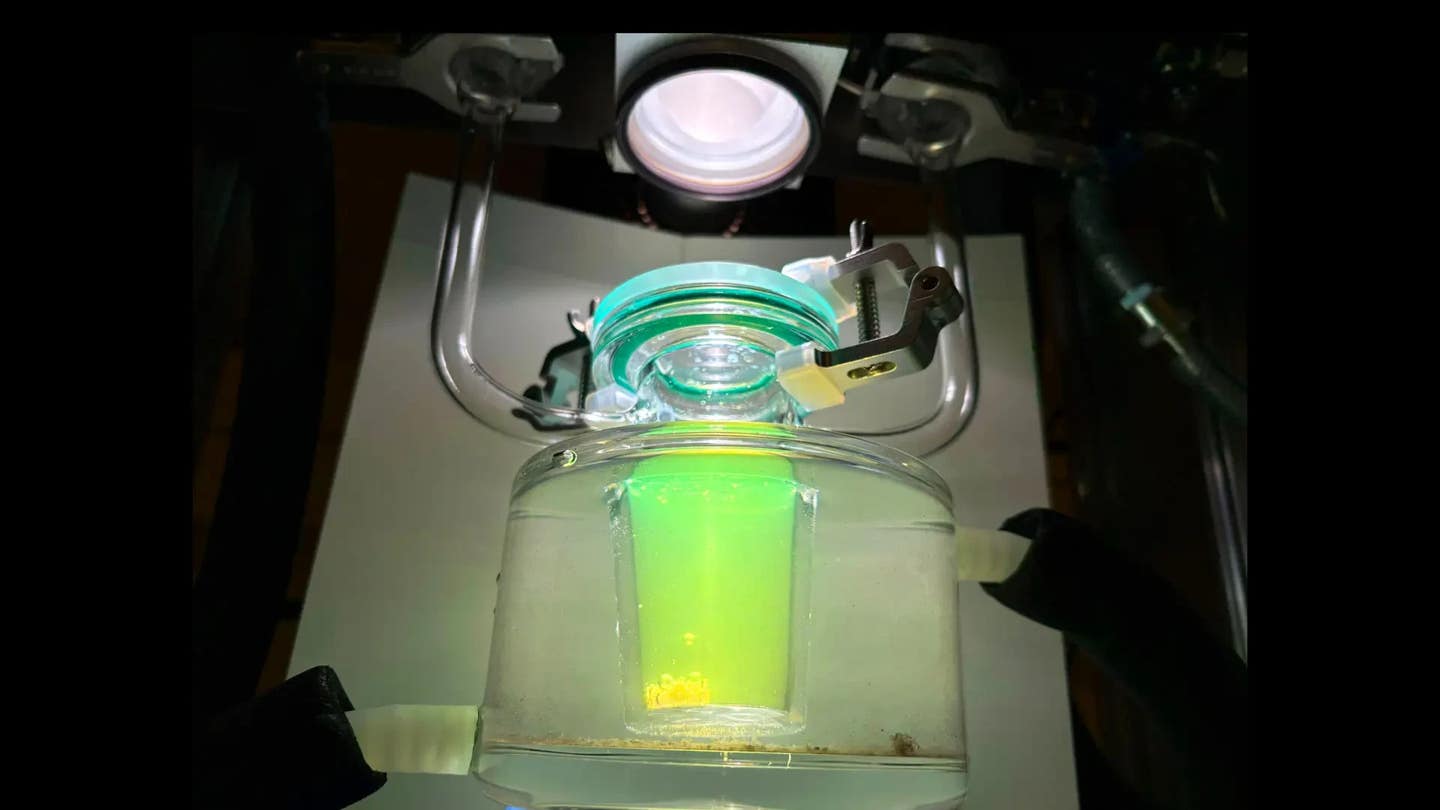
A groundbreaking gel treatment for middle ear infections eliminates antibiotics’ side effects and antibiotic resistance. (CREDIT: CC BY-SA 4.0)
Middle ear infections are common, painful, and frustrating, especially for young children and their parents. Antibiotics prescribed orally often trigger side effects, lead to repeat infections, and increase antibiotic resistance.
Scientists from Cornell University, led by researchers Rong Yang and Wenjing Tang, have developed a new topical gel that cures ear infections effectively with just a single application, offering relief without the typical drawbacks.
A Common Childhood Problem
Acute otitis media (AOM) is the most frequent reason doctors prescribe antibiotics for children. It accounts for more than half of all pediatric antibiotic prescriptions worldwide. Around 80% of kids experience at least one ear infection before age three. In the U.S. alone, ear infections lead to over 15.8 million cases each year, costing approximately $4.3 billion annually.
AOM occurs when bacteria or viruses invade the fluid-filled space behind the eardrum. The leading bacterial culprits include Streptococcus pneumoniae, Moraxella catarrhalis, and increasingly, Haemophilus influenzae, which has become tougher to treat after widespread use of the pneumococcal vaccine.
Current treatments typically involve high doses of oral antibiotics, usually amoxicillin, taken for up to 10 days. While effective, these medications can cause uncomfortable side effects like stomach upset, yeast infections, and allergic reactions. More seriously, frequent antibiotic use contributes significantly to global antibiotic resistance.
Adding urgency to the problem, a national shortage of liquid amoxicillin recently highlighted how vulnerable current treatments are to supply disruptions. To tackle these challenges, scientists are actively seeking treatments that cut antibiotic use without compromising effectiveness.
Related Stories
Overcoming the Eardrum Barrier
Directly applying antibiotics to the infected area behind the eardrum would minimize side effects and lower antibiotic use. However, the eardrum itself—a thin membrane about 100 micrometers thick—is extremely resistant to penetration by most medications.
Previously, chemical agents were used to break down the eardrum's protective layer temporarily, allowing medicine to pass through. Unfortunately, these chemicals often cause skin irritation or allergic reactions, severely limiting their practical use.
The Cornell researchers decided to take a different approach. They developed tiny particles called liposomes—bubble-like structures made of fats—to encapsulate antibiotics. Liposomes have been successfully used since the 1980s to deliver medications across the skin safely. Yet, designing liposomes specifically for crossing the eardrum has been a challenge because previous assumptions about their optimal properties proved incorrect.
The Surprising Success of Negative Charges
Earlier studies suggested positively charged liposomes worked best to cross healthy skin, as they bind strongly to the negatively charged surface of skin cells. Surprisingly, the Cornell team's experiments revealed that negatively charged liposomes perform much better during active ear infections.
To test their hypothesis, researchers created two types of antibiotic gels, one with negatively charged liposomes and another with positively charged ones. Both contained the antibiotic ciprofloxacin, often used for ear infections. They applied these gels to infected chinchillas—animals whose ears closely resemble human ears—and compared the outcomes.
The results were clear: the negatively charged liposomes cured 100% of infections within 24 hours. In contrast, positively charged liposomes only worked half the time, and gels with antibiotic alone cured only 25%. Moreover, animals treated with the negatively charged liposome formulation experienced no inflammation or reinfection during the seven-day observation period.
Why Negative Charges Worked Better
Yang and Tang's team discovered why negatively charged liposomes outperformed positively charged ones during infections. Infected ears activate the body's immune response, especially the complement system—a group of proteins that helps immune cells recognize and capture invading pathogens. Negatively charged liposomes effectively attracted these immune cells, which then carried the antibiotic directly into the infected area.
"A single-dose treatment for middle ear infections represents a significant step forward toward reducing the burden on families and improving outcomes for young children," explained Yang. By leveraging the body's own immune response, the researchers achieved highly efficient drug delivery across the eardrum.
Practical and Safe Application
The antibiotic gel developed by Yang's group is simple and practical for pediatricians to use. Doctors could apply a single dose through the outer ear canal during a regular office visit. This gel solidifies quickly, slowly releasing medication over seven days. This method drastically cuts the antibiotic dose—from the standard 675 mg per kilogram body weight down to just 2 mg.
Parents have already shown significant interest. "I often receive emails from parents asking when our formulation will be available, and I share their hope for a solution," said Yang. The new method not only promises relief from pain and infection but also helps prevent long-term antibiotic resistance, a global health priority.
Next Steps Towards Clinical Use
The researchers are eager to translate their lab success into clinical reality. According to Yang, the next stage involves rigorous testing and approvals needed to bring this innovative treatment to pediatric clinics everywhere. “I am most excited about translating this technology from the lab to the clinic," Yang said, "as it has the potential to improve patient compliance, reduce antibiotic resistance, and ultimately transform how children receive antibiotics."
This breakthrough represents more than just improved treatment for a common childhood ailment. It could reshape the way antibiotics are prescribed globally, offering relief to millions of children and peace of mind to their parents.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.