Groundbreaking treatment uses programmed bacteria to kill cancer cells
For the past few years, scientists have celebrated the potential of CAR-T cells in treating specific types of blood cancers, namely leukemia
[Nov. 1, 2023: Staff Writer, The Brighter Side of News]
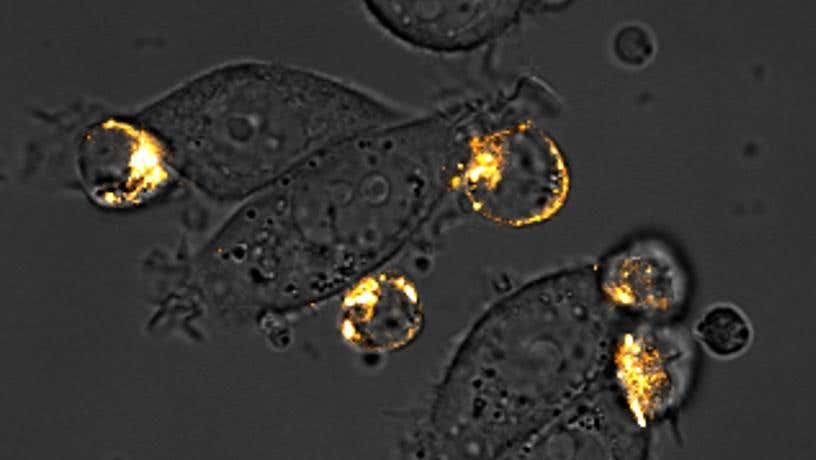
Microscopy image of CAR-T cells attacking ‘painted’ breast cancer cells. (CREDIT: Rosa Vincent and Thomas Savage/Columbia Engineering)
For the past few years, scientists have celebrated the potential of CAR-T cells (chimeric antigen receptor T cells) in treating specific types of blood cancers, namely leukemia and lymphoma. These cells are engineered to latch onto and destroy specific markers (antigens) found on the cancerous blood cells.
However, the same success hasn't been translated to solid tumors like those in breast and colon cancers.
Solid tumors present a more complex landscape as they comprise a blend of cells with varying antigens, many of which can be identical to those found on healthy cells. This has made it particularly challenging to find a reliable target for CAR-T cell therapy, with many attempts stalling in the initial stages.
Programmed bacteria acts as beacons that guide engineered T cells to destroy cancer cells in solid tumors. (Credit: Synthetic Biological Systems Laboratory/Columbia Engineering)
Yet, in a groundbreaking announcement today, scientists from Columbia Engineering have illuminated a hopeful path forward.
A Revolutionary Cancer Combat Strategy
Tal Danino, associate professor of biomedical engineering, along with his dedicated team, has unveiled a trailblazing method to counteract these solid tumors. They've ingeniously engineered probiotics, which are often referred to as "friendly bacteria", to target and invade these tumors. Once there, these bacteria generate synthetic markers, making the tumor cells more recognizable to CAR-T cells which then proceed to eliminate them.
Related Stories
Elaborating on this achievement, Danino explained, “Our probiotic platform enables CAR-T cells to attack a broad range of tumor types.” He further added, “Traditional CAR-T therapies have relied on targeting natural tumor antigens. But now, we're pairing engineered T cells with engineered bacteria to pinpoint synthetic antigens in solid tumors. The potential implications for cancer treatment are monumental.”
By leveraging this strategy, Danino's laboratory has ushered in the era of a "universal" CAR-T cell. This cell aims at a universal marker by guiding the bacteria to tag solid tumors with a synthetic marker. It’s hoped that as this research matures, it might eliminate the need to pinpoint a unique tumor antigen and craft a unique CAR-T cell therapy for each cancer variant and patient, streamlining the process significantly.
A Leap in Medical Innovation
This cutting-edge ProCAR platform, where probiotics guide CAR-T cells, isn't just a mere combination of the two. It's the first instance where such a synergy has resulted in CAR-T cells reacting to synthetic antigens produced within the tumor itself.
Engineered E. coli Nissle 1917 (EcN) produces GFP-based CAR targets and engineered triple negative breast cancer (TNBC) cells express cell surface GFP. (CREDIT: Science)
Rosa Vincent, a doctoral student in Danino’s team and co-lead author of the study, commented on this innovation. “We envisioned a merger between the individual strengths of two cell therapies,” she said. “The bacteria play the role of the marker, and the T cells then move in for the elimination of the harmful cells.”
Promise in Preliminary Findings
Their research has showcased promising results in various models of human and mouse cancers. Human T cells, in particular, seemed to thrive in the presence of these engineered bacteria within the tumor, amplifying their ability to counteract cancer cells.
His-tag purified ‘Tag’-GFP binds to collagen coated plates and strongly activates GFP CAR+ Jurkats. Plasmid map of protein expression vector transformed into Nico cells for protein purification of dimeric (diGFP) and Tag sfGFP variants. (CREDIT: Science)
Summing up their work, Danino said, “Our ProCAR platform offers a novel method to amplify CAR-T cell therapy's impact on solid tumors. Though we're still deep in the research phase, we're excited about the possibilities this could bring to cancer treatment.”
What Lies Ahead
This groundbreaking work didn't occur in isolation but was part of an extensive collaborative effort with the laboratory of Nicholas Arpaia at Columbia’s Vagelos College of Physicians and Surgeons. Both teams have previously joined forces in developing bacteria that can deliver immunotherapy treatments.
Tag stains a significantly reduced population of immune effector cells relative to CT26 tumor cells. (CREDIT: Science)
Energized by their current findings, the researchers are committed to refining their methods. They have their sights set on initiating clinical trials, keen to explore this platform's safety and effectiveness in treating human patients.
As science pushes its boundaries, such innovative strategies give renewed hope to millions affected by cancer, offering the prospect of more efficient and versatile treatments on the horizon.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.