Gut molecule TMA improves blood sugar control and blocks inflammation linked to diabetes
Researchers find a gut-made chemical blocks inflammation and improves blood sugar, opening new paths for treating insulin resistance.

 Edited By: Joseph Shavit
Edited By: Joseph Shavit
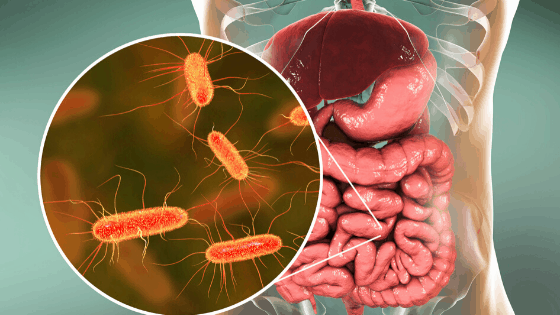
A molecule made by gut bacteria acts like a medicine, blocking a key immune trigger and improving blood sugar control in new research. (CREDIT: Wikimedia / CC BY-SA 4.0)
Diabetes now affects about 529 million people worldwide, and roughly 1.6 million die from it each year. At the center of the crisis is insulin resistance, a condition in which your cells stop responding well to insulin. This failure raises blood sugar and increases the risk of heart disease. Sedentary habits, processed foods and rising obesity have fueled a steady global climb in the disorder.
A quieter driver worsens the problem. Long-lasting, low-grade inflammation moves through the body and interferes with how insulin works. Fats in food, changes in gut bacteria and immune signals combine to keep that inflammation alive. Bacterial fragments and fatty acids can trigger a receptor called TLR4, which links the immune system with blood sugar control. Scientists call this process metabolic endotoxemia because events in the gut shape disease far beyond the intestine.
For years, researchers suspected that small chemicals made by microbes act as messengers to human cells. Many bind to receptors on cell surfaces or inside the nucleus. Yet some scientists believed these microbial products might also target kinases, proteins that flip cellular switches controlling growth and immunity. A new study now confirms that idea with striking clarity.
An international team led by Professor Marc-Emmanuel Dumas at Imperial College London and CNRS, with Professor Patrice Cani at Imperial College London and the University of Louvain, Dr. Dominique Gauguier at Imperial and INSERM in Paris and Professor Peter Liu at the University of Ottawa Heart Institute, reports that a gut-derived molecule behaves like a drug. The compound, trimethylamine or TMA, blocks a critical immune kinase called IRAK4. The work appears in the journal Nature Metabolism.
A Clue Hidden in Diet and Microbes
The story reaches back two decades. As a postdoctoral scientist, Cani found that a high-fat diet allowed bacterial components to enter the body and spark inflammation that promoted insulin resistance. Many thought the idea far-fetched in 2005. It is now mainstream biology.
The latest study began with mice fed either standard food or a diet in which fat supplied most calories. Those on the fatty menu developed obesity and trouble handling sugar. Surprisingly, classic signs of liver inflammation did not rise as expected. The team then checked urine metabolites and noticed something unusual. Mice on the high-fat diet excreted far more TMA, a chemical made when microbes break down nutrients like choline and carnitine.
That finding raised a question. Could TMA be linked to the strange lack of liver inflammation? To find out, the scientists enriched the high-fat diet with extra choline. Sugar control improved, weight gain slowed and blood markers of inflammation fell. TMA in the blood climbed about twenty-fold. The pattern pointed to one suspect.
When the Messenger Is Silenced
Proof came from shutting TMA down. The researchers used antibiotics and a precision blocker to stop microbes from making it. Once TMA vanished, choline lost its benefits. Blood sugar worsened and key insulin signals in the liver failed to recover. Weight did not change much, which showed that TMA worked through immunity and metabolism rather than appetite alone.
Then came the reverse test. The team delivered TMA directly to mice on the low-choline, high-fat diet. Extra TMA restored normal sugar handling and cut inflammatory signals in the blood and liver. Weight still held steady. The molecule alone could mimic the effects of choline.
What target could explain such power? The scientists screened hundreds of kinases in the human kinome. Only one stood out. TMA bound tightly to IRAK4, a protein that helps transmit alarms from TLR4. In lab tests, TMA shut down IRAK4’s activity at levels similar to those seen in living animals.
The group then tested human immune cells. When exposed to bacterial toxins, the cells released far less IL-6 and TNF if pretreated with TMA. A specific IRAK4 drug produced the same result. Other immune triggers still worked, showing that TMA does not silence defense broadly. It acts through a narrow channel.
From Molecular Target to Living Proof
Results in whole animals matched those in cells. Mice facing a lethal dose of bacterial toxin survived more often after receiving TMA, much like animals bred without active IRAK4. In human liver cells exposed to a damaging fatty acid, TMA blocked inflammatory steps and protected insulin signaling.
Genetics added another layer. Mice lacking IRAK4 fared better on fatty food even without extra choline. They kept steadier blood sugar and produced fewer inflammatory proteins. Finally, treating animals with the IRAK4 drug improved weight, sugar control and liver function. Every path led to the same mechanism.
The implications extend beyond a single molecule. TMA comes from everyday nutrients in eggs, fish and some meats. It is later converted in the liver to TMAO, a compound tied to heart risk in some studies. The authors stress that balance matters. Their work shows that TMA itself can dampen harmful inflammation. Adjusting the shift between TMA and TMAO or targeting IRAK4 directly could open a new class of therapies.
“This shows how nutrition and our gut microbes can work together by producing molecules that fight inflammation and improve metabolic health!” said Cani.
Dumas added, “We’ve shown that a molecule from our gut microbes can actually protect against the harmful effects of a poor diet through a new mechanism. It’s a new way of thinking about how the microbiome influences our health.”
Practical Implications of the Research
The findings point to two near-term paths for treatment. One is drug therapy. IRAK4 inhibitors already exist for other diseases. Repurposing them could speed clinical trials for insulin resistance.
The second path is dietary and microbiome design. Scientists can explore foods, supplements or probiotics that raise helpful TMA signals without increasing heart risk. Long term, this could lead to personalized diets tuned to a person’s gut chemistry.
For the public, the work highlights that what you eat does more than feed you. It also trains your microbes to send signals that can heal or harm. Understanding that dialogue may help prevent diabetes rather than treat it after damage sets in.
Research findings are available online in the journal Nature Metabolism.
Related Stories
- Scientists discover a hidden connection between type 2 diabetes and hearing loss
- Low-dose aspirin can reduce risk for heart attacks and strokes in adults with Type 2 diabetes
- You can prevent type 2 diabetes without losing weight, study finds
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Writer and Editor
Joshua Shavit is a Nor Cal-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a co-founder of The Brighter Side of News, he focuses on positive and transformative advancements in technology, physics, engineering, robotics and astronomy. Joshua's work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.