Lifechanging study reveals that damaged nerves can be regenerated
Novel technique called interventional cryoneurolysis has emerged as a potential game-changer for patients suffering from chronic nerve pain
[Nov. 18, 2023: JJ Shavit, The Brighter Side of News]
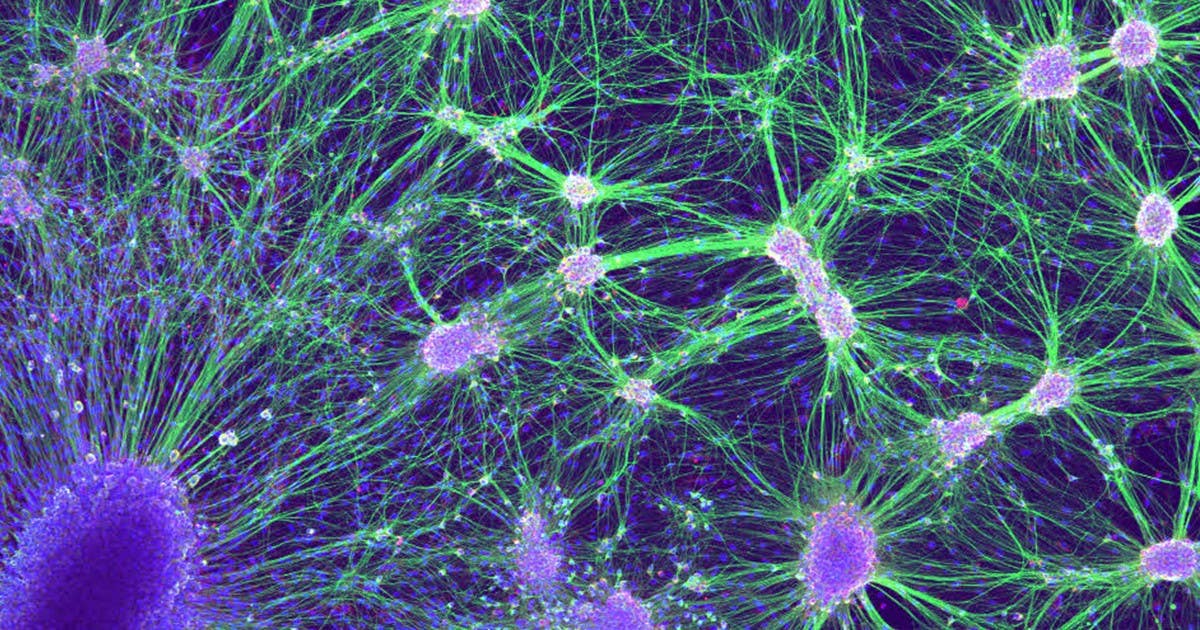
Damaged nerves can be regenerated with the application of a frozen needle under advanced imaging guidance. (CREDIT: Creative Commons)
In a groundbreaking development in the field of interventional radiology, a novel technique called interventional cryoneurolysis has emerged as a potential game-changer for patients suffering from chronic nerve pain. This innovative approach, which involves the precise application of a frozen needle under advanced imaging guidance, has shown remarkable success in regenerating damaged nerves.
Researchers from Emory University, led by Dr. J. David Prologo, have presented their findings on this promising technique at the Society of Interventional Radiology Annual Scientific Meeting in Boston, offering new hope to individuals enduring persistent pain following traumatic injuries.
The Quest for Alternatives to Opioids
The opioid epidemic in the United States has prompted a critical need for alternative pain management strategies. Dr. Prologo, an interventional radiologist and associate professor at Emory University School of Medicine in Atlanta, emphasized the importance of exploring non-opioid options for pain relief.
He stated, "The idea that we can induce regeneration of damaged nerves simply by placing a cold needle through the skin under imaging guidance is extremely exciting." This approach aligns with the call from United States legislators and medical societies to develop alternatives to opioids for managing pain.
The Science Behind Cryoneurolysis
The core of the interventional cryoneurolysis technique lies in the precise use of advanced imaging, such as CT-guidance, to target damaged nerves with a freezing needle. When executed accurately, the cold temperature causes the damaged nerves to degenerate and lose function. Dr. Prologo explained, "What happens next is almost magical. If the nerve is exposed to the correct amount of cold, over the correct area, for the right amount of time, it will regenerate—replacing the previously damaged nerve with a healthy one."
Related Stories:
The study conducted at Emory University involved treating eight patients who had been suffering from chronic nerve pain resulting from previous traumatic injuries. Remarkably, the average time between the traumatic event and the interventional cryoneurolysis procedure was 9.5 years. Importantly, the researchers reported no procedure-related complications or adverse events. Furthermore, all patients experienced a return to their baseline strength over time, confirming the regeneration of the targeted nerve.
Perhaps the most significant result of this study was the substantial improvement in pain symptoms observed in six of the eight patients. This improvement was quantified through a collective decrease of 4.6 points in Visual Analog Scale (VAS) pain scores, a widely used tool for measuring pain intensity.
Dr. Prologo is enthusiastic about the potential of interventional cryoneurolysis to revolutionize pain management. He highlighted the diverse range of conditions that could benefit from this technique, stating, "Interventional radiologists can place these needles safely in precise locations all over the body, allowing access to pain generators that were previously unreachable and giving hope to patients who struggle with pain."
Cryoneurolysis: How I Do It. (CREDIT: J. David Prologo, MD, FSIR, ABOM-D)
This technique not only has the potential to address nerve pain induced by trauma but also offers promise for conditions such as pudendal neuralgia, post-mastectomy pain, post-surgical pain, and more, historically managed with narcotics.
Understanding the Visual Analog Scale (VAS)
To assess the effectiveness of the interventional cryoneurolysis technique, researchers relied on the Visual Analog Scale (VAS) to measure pain intensity. The VAS is a pain rating scale introduced in 1921 by Hayes and Patterson and has since become a valuable tool in epidemiological and clinical research for evaluating the intensity or frequency of various symptoms.
The VAS represents a continuum of pain intensity, ranging from none to an extreme amount of pain. Unlike discrete categorizations like none, mild, moderate, and severe, the VAS captures the concept of an underlying continuum of pain intensity as perceived by patients.
The primary purpose of the VAS is to provide a unidimensional measure of pain intensity. It enables healthcare professionals to record the progression of a patient's pain over time or to compare pain severity among individuals with similar conditions. The VAS has been widely utilized in various adult populations, including those with rheumatic diseases, chronic pain, cancer, and allergic rhinitis. Beyond assessing pain, it has also been employed to evaluate mood, appetite, asthma, dyspepsia, ambulation, and disease control.
The VAS can be presented in different formats, including numerical rating scales, curvilinear analog scales, box-scales with circles, graphic rating scales, and Likert scales with descriptive terms along a line. The most common format consists of a straight horizontal line, typically 100 millimeters in length, with the extreme limits of the parameter being measured defined at the ends. In some studies, horizontal scales may be oriented from right to left, while others use vertical VAS.
Researchers have found no significant difference in the effectiveness of horizontal and vertical VAS. However, the choice of terms to define the scale's anchors, such as the left (worst) and right (best) ends, is considered crucial to ensure accurate and reliable measurements.
With no procedure-related complications and a substantial reduction in pain intensity measured using the Visual Analog Scale, this groundbreaking approach may indeed revolutionize pain management, providing a much-needed alternative to opioids.
As research in this field continues to evolve, interventional cryoneurolysis could potentially transform the lives of individuals battling chronic pain and pave the way for further applications in pain management across various medical conditions.
Note: Materials provided by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Joseph Shavit
Head Science News Writer | Communicating Innovation & Discovery
Based in Los Angeles, Joseph Shavit is an accomplished science journalist, head science news writer and co-founder at The Brighter Side of News, where he translates cutting-edge discoveries into compelling stories for a broad audience. With a strong background spanning science, business, product management, media leadership, and entrepreneurship, Joseph brings a unique perspective to science communication. His expertise allows him to uncover the intersection of technological advancements and market potential, shedding light on how groundbreaking research evolves into transformative products and industries.
