Man injected by 856 snake bites helps create universal antivenom
A universal snake antivenom might soon be within reach—thanks to one man’s strange and dangerous obsession. For nearly two decades, Tim Friede has deliberately injected himself with venom from some…

Tim Friede’s extreme self-immunization helped researchers craft a breakthrough universal antivenom that protects against 19 deadly snake species. (CREDIT: CC BY-SA 4.0)
A universal snake antivenom might soon be within reach—thanks to one man’s strange and dangerous obsession. For nearly two decades, Tim Friede has deliberately injected himself with venom from some of the world’s deadliest snakes.
His purpose wasn’t fame or shock value, although his YouTube videos certainly caught attention. It was to build immunity—and it worked. His extreme exposure triggered his body to produce rare and powerful antibodies. Now, researchers have turned those antibodies into a promising new treatment that could save tens of thousands of lives every year.
A Neglected Global Killer
Snake envenomation ranks among the world’s deadliest neglected tropical diseases. Each year, venomous snakes cause between 100,000 and 138,000 deaths and leave over 300,000 survivors with lasting disabilities. Most of these cases occur in poor, rural areas across Africa, Asia, and Latin America, where access to proper medical treatment is limited.
Despite the severity of the problem, treatments haven’t evolved much in over a century. Antivenoms are still mostly produced by injecting horses or sheep with snake venom, then harvesting the animals’ antibodies. These traditional serums work—but they come with serious drawbacks. They’re often species-specific, meaning the venom and antivenom must match.
That’s a huge issue when victims can’t identify the snake. Reactions to the non-human proteins also range from uncomfortable to dangerous, and modern digestion of antibodies to reduce risks often shortens their effectiveness. On top of this, many antivenoms are contaminated with non-antibody proteins and often contain only a small fraction—sometimes just 9 to 15 percent—of venom-specific antibodies.
Making things worse, the venom of a single snake species can vary based on its geographic region. Some areas lack any effective antivenom at all. The need for better, broader protection has never been more urgent.
Related Stories
Building a Better Antivenom
For years, scientists struggled to create a universal antivenom. The challenge stems from nature itself: over 600 venomous snake species have evolved for 167 million years. Each species can produce between 5 and 70 unique protein toxins.
The most dangerous group—elapids, which includes cobras, mambas, and kraits—are especially complex. Their venoms are mostly made up of three-finger toxins (3FTXs) and phospholipase A2 (PLA2) enzymes. The 3FTXs fall into two major types: long-chain (LNXs) and short-chain neurotoxins (SNXs). Both interfere with the nervous system by binding to nicotinic acetylcholine receptors (nAChRs), causing paralysis and often death.
Despite their diversity, these toxins share a key weakness. To block nerve signals across species, their structure must remain similar enough to bind nAChRs with high affinity. That evolutionary constraint made them ideal targets for scientists trying to create a broad-spectrum therapy.
The Man Who Made Himself Immune
That’s where Tim Friede enters the story. Starting in 2001, the Wisconsin native exposed himself to snake venom 856 times over 18 years. Sometimes he used syringes. Other times he let the snakes bite him. His list included black mambas, king cobras, taipans, rattlesnakes, and more. On one occasion, he nearly died after receiving two cobra bites in a single hour. But through sheer persistence, Friede’s immune system learned to survive what would normally kill a horse.
His efforts didn’t go unnoticed. Jacob Glanville, a computational immune engineer and CEO of the biotech firm Centivax, saw the videos and recognized the potential. He reached out, and Friede became the cornerstone of a groundbreaking study published in the journal Cell.
“We identified a hyperimmune human adult male donor with a documented 18-year history of self-immunizations,” Glanville said. “Not only did he potentially create these broadly neutralizing antibodies, in this case, it could give rise to a broad-spectrum or universal antivenom.”
Crafting the Antivenom Cocktail
The team at Centivax isolated antibodies from Friede’s memory B cells—the immune system’s long-term record-keepers. Using an “iterative-addition” approach, they focused on neutralizing the core components of elapid venom. First, they extracted two antibodies. One, named LNX-D09, targets long-chain neurotoxins. The other, SNX-B03, neutralizes short-chain ones. These were then paired with a small-molecule inhibitor known as varespladib, which blocks PLA2 enzymes.
Together, this three-part cocktail was tested on mice exposed to venom from 19 of the world’s most medically important elapid species. Thirteen of the venoms were fully neutralized, with the mice surviving entirely. The remaining six showed partial protection.
That breadth of protection was unprecedented. “By the time we reached three components, we had a dramatically unparalleled breadth of full protection,” Glanville explained.
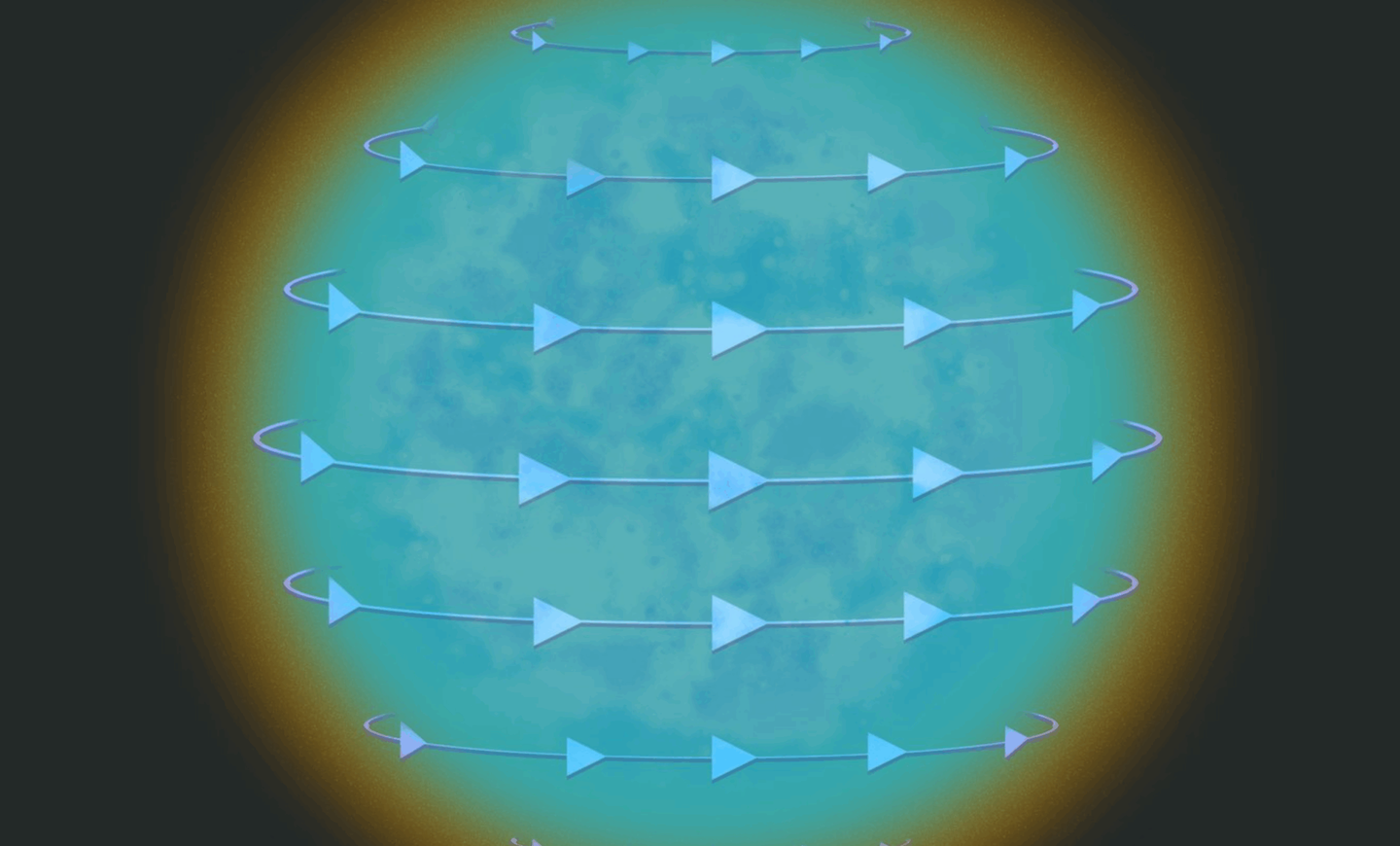
Crystal structure analysis confirmed the antibodies were mimicking the exact binding interfaces between the toxins and the nAChRs. This mimicry allowed the antibodies to lock onto the venom toxins before they could reach the receptors, neutralizing their effects.
One Cocktail, Many Snakes
The 19 species tested included some of the deadliest snakes known: king cobras, black mambas, tiger snakes, and others. All fall under WHO Categories 1 and 2—snakes considered highly dangerous to humans. The success of the three-component treatment marks a major step toward creating a universal antivenom.
“This could eliminate the need for snake species identification as a prerequisite for treatment,” Glanville said. “It would provide coverage for many of the 650 venomous snake species, even in regions with no existing antivenom.”
While other efforts to create broadly effective antibodies have been made before, they either showed only partial results or failed to protect against whole venoms. Some used synthetic yeast libraries or computational designs. Others protected only against isolated toxins or a single cobra species. But none provided the range or in vivo protection shown here.
What’s Next?
The current cocktail targets the elapid family, which includes over 300 species across 50 genera. It may protect against untested species in the same family, but another major goal remains: the vipers. These snakes, such as rattlesnakes and puff adders, belong to a different family with different venom profiles.
“We're turning the crank now,” said co-author and Columbia University biochemist Peter Kwong. “We're going through the same process to find the minimum sufficient cocktail to protect against viper venom.”
Before this universal antivenom can reach hospitals, it must pass rigorous clinical trials. For now, researchers plan to begin testing the cocktail on dogs bitten by snakes in Australian veterinary clinics. If those trials go well, human trials will follow.
The potential impact is huge. A single, human-derived, pan-antivenom could save lives in regions with limited healthcare access, reduce the cost of treatment, and simplify first aid for travelers and rural workers alike.
And to think—it all started with one man, a handful of snakes, and an immune system forged in venom.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.