New AI model discovers two proteins that work together to prevent Crohn’s disease
Scientists uncover how GIV and NOD2 proteins keep gut inflammation in check, revealing new targets for Crohn’s therapy.

 Edited By: Joseph Shavit
Edited By: Joseph Shavit

UC San Diego researchers used AI and molecular biology to uncover how two proteins, GIV and NOD2, work together to prevent Crohn’s disease. (CREDIT: Shutterstock)
Your gut harbors trillions of microbes which live in precarious harmony with your immune system. When that harmony is upset, the results can be excruciating—especially for those with Crohn's disease, a long-term inflammatory bowel disorder. Scientists at the University of California San Diego School of Medicine have now uncovered how two key proteins work together to maintain that equilibrium—and what happens when their partnership falters.
The gut's immune defense depends on two types of cells called macrophages. They possess one that comes in to kill nasty bacteria and one that repairs injured tissue and calms down inflammation after danger has been removed. In Crohn's disease, that teamwork breaks down. Inflammatory macrophages take over, resulting in chronic inflammation, tissue loss, and severe belly pain.
Researchers have known for a long time that mutations in one gene called NOD2 increase the risk of Crohn's but did not know the full reason why. Dr. Pradipta Ghosh and her research team went to artificial intelligence and new molecular technology to unravel the enigma.
A Critical Partnership: NOD2 and GIV
NOD2 is a gut immune system's vigilant eye. It senses fragments of bacteria—cues of infection to come—and helps macrophages destroy germs while tempering inflammation so that it won't get out of control. But in the majority of Crohn's patients, this system breaks down.
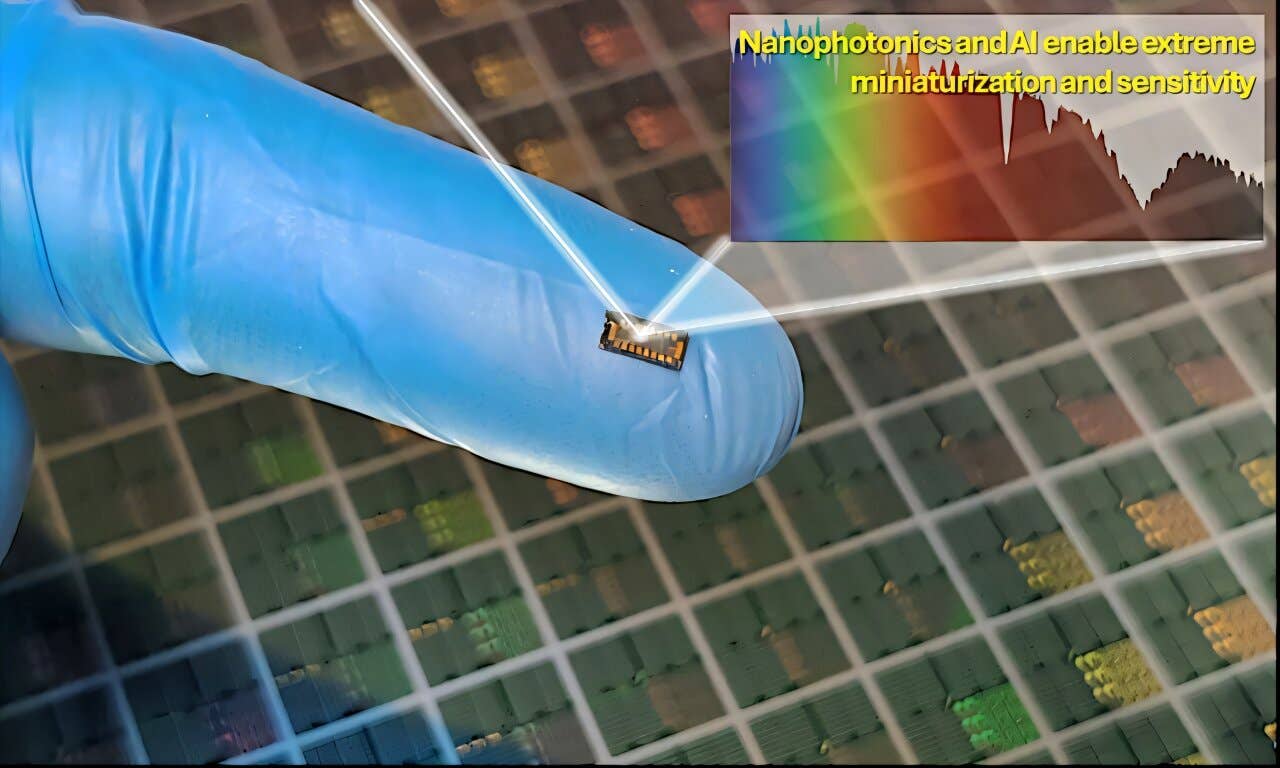
To find out why, the UC San Diego researchers trained a machine learning algorithm to contrast activity in inflamed versus normal colon tissue macrophages. Among thousands of genes, they found 53 that determine whether a macrophage takes on an inflammatory or healing role. One gene stood out—it produces a protein named girdin (GIV), which helps cells communicate with each other.
The scientists determined that GIV directly attaches to NOD2 within healthy cells through a region of NOD2 known as the leucine-rich repeat, or LRR. Both GIV and NOD2 collaborate to contain inflammation. But in people with a common NOD2 mutation, that LRR domain is not present—so GIV can't attach. Without this bond, inflammation spirals out of control.
"NOD2 is the body's infection surveillance system," Ghosh explained. "When combined with girdin, it maintains gut immunity in check. Without that combination, the system collapses."
When the System Breaks Down
To determine, researchers studied mice that lacked GIV and compared them to normal mice. When exposed to gut bacteria, the mice lacking GIV became wildly inflamed, developed thickened intestines, and tissue scarring—all the same symptoms as human Crohn's. Multiple ones also developed sepsis, a potentially fatal, body-wide immune response.
Dr. Gajanan D. Katkar, the co-first author of the study, compared the gut to "a battlefield" where macrophages are like peacekeepers. "AI has enabled us to track players from both sides for the first time with clarity," he said.
Microscopy photographs confirmed that GIV and NOD2 accumulate in groups within macrophages shortly after they encounter bacteria. Those groups show up at locations where the cell's actin filaments and mitochondria, its energy sources, are concentrated. In the absence of GIV, those groups never form, leaving macrophages helpless against bacteria and causing the immune system to attack healthy tissue instead.
How AI Helped Unravel the Mystery
By combining AI analysis of data with lab and animal research, the UC San Diego scientists closed one of Crohn's disease's longest-standing mysteries. In their published paper in the Journal of Clinical Investigation, they show that interfering with the GIV–NOD2 interaction triggers a chain reaction of runaway inflammation.
In normal times, this cooperation helps macrophages shift from battle to healing when infection subsides. Without GIV, that shift never takes place—healing genes are dormant while inflammatory genes are active. The immune response never gets the signal to stand down.
The study also tells us about how people with the NOD2 1007fs mutation, among the most common risk factors for Crohn's, are hit the hardest. The mutation removes the exact spot GIV needs to bind onto, making NOD2 incapable of controlling inflammation. Gut bacteria are thrown off balance and tissue repair is halted.
When researchers treated healthy mice with bacterial fragments that activate NOD2, the mice were protected against tissue damage and inflammation. But the treatment did not benefit GIV-deficient mice—proof that the benefits of NOD2 depend entirely on its interaction with GIV.
A New Way Forward for Crohn's Treatment
Crohn's medication today eliminates the entire immune system, putting patients at greater risk of infection. The UC San Diego breakthrough hints at a wiser approach—to revive the normal GIV–NOD2 association instead of squashing immunity altogether.
The researchers suggest that GIV-mimetic drugs might one day prevent flares. Because their mouse model develops Crohn's-like disease within seven weeks, it might also accelerate testing for new treatments.
Beyond the Gut
This discovery doesn't just shed light on Crohn's disease—it brings to light how immune cells all over the body achieve balance between destruction and repair.
An understanding of this partnership can lead to treatments for numerous autoimmune diseases that can benefit millions of people afflicted with chronic inflammation.
Research findings are available online in the Journal of Clinical Investigation.
Related Stories
- The surprising science behind flatulence and gut health
- Revolutionary molecule combats autoimmune diseases, including lupus and Crohn’s disease
- New T cell protein discovery stops autoimmune diseases in their tracks
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Shy Cohen
Writer