New antibody restores immune system to fight pancreatic cancer
Scientists uncover a sugar shield that helps pancreatic tumors evade immunity and develop an antibody that reactivates macrophages.

 Edited By: Joshua Shavit
Edited By: Joshua Shavit
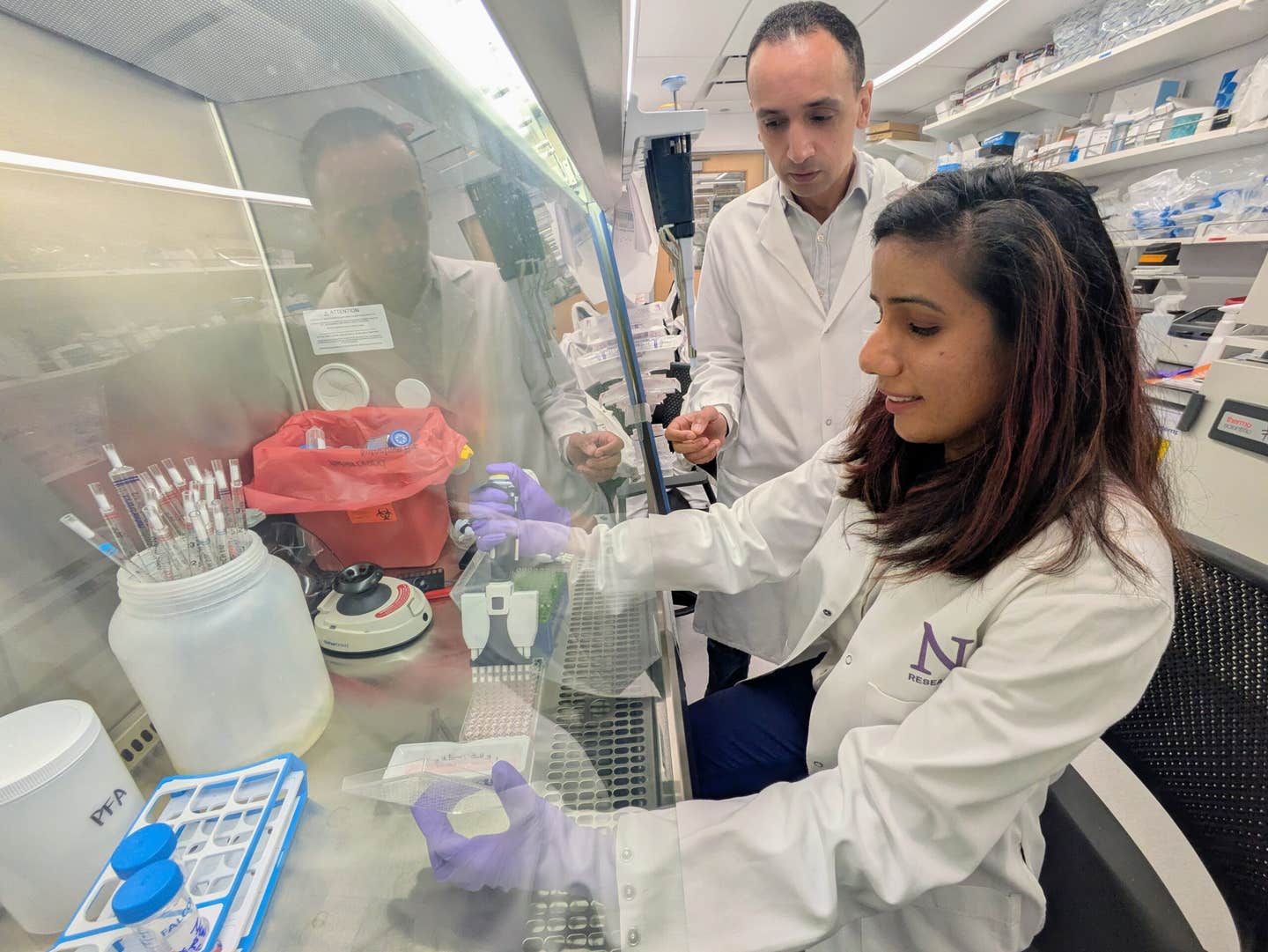
Sugar shield on pancreatic tumors reveals new path for immune-based treatment. Study authors Abdel-Mohsen and Saini in Abdel-Mohsen’s lab. (CREDIT: Northwestern University)
Survival rarely comes easy when pancreatic ductal adenocarcinoma strikes. Most people learn of it only after it has spread, and only a small fraction reach the five-year mark. Treatments that succeed against other cancers often fall short here. Many scientists believe the reason lies in the tumor’s surrounding environment, where immune cells and cancer cells crowd together in a tense and unbalanced standoff.
How a Natural Warning System Goes Awry
Inside this small compartment, immune cells called macrophages should act as the sergeant guard cats. They ordinarily function to clear dead cells, debris and stay on patrol, to promote healthy tissue. But in pancreatic carcinoma, macrophages become repressed and abandon their protective drive to attack tumors. The consumption of the cancer cells, a function referred to as phagocytosis, is also diminished.
For a long time, researchers have been attempting to re-engage these cells. Most focus has been given to a protein called CD47 that sends a "do not eat me" signal when it binds to specific macrophage receptors. Blocking CD47 has implications for a few cancers, but pancreatic tumors have been slow to respond to progress. The attention of the investigators led to questions that go deeper than just one receptor.
Complex World of Sugars
And now their attention turned to the more complex world of sugars displayed on the surface of cells called glycans. Many cells have sugar molecules on them, called glycans. When tumors rearrange or upregulate these sugars, they can initiate sensory fraud changes in the immune system.
One of these sugars is a common sugar called sialic acid. Sialic acid gives the glycans that it is attached to the ability to bind and silence a receptor code-named Siglecs displayed on macrophages. Once bound, Siglecs send a message internally to tell the macrophage to stand down.
Prior investigations in breast and ovarian tumors demonstrated that Siglec-10 engages with a glycoprotein named CD24, and interference with CD24 enhances the ability of macrophages to defend against those tumors. The question arose as to whether a similar system was evident in pancreatic tumors.
The Sugar Coating That Masks A Glycoprotein Key
Scientists utilized publicly available genetic information to identify that Siglec-10 expression was higher in pancreatic tumors as compared to normal tissue, but CD24 was not selectively elevated. Instead, multiple genes involved in sialic acid-rich glycan constructions were upregulated, indicating pancreatic tumors potentially utilize an alternative sugar-decorated glycoprotein to silence Siglec-10.
The scientists cultured human macrophages with fluorescently labeled pancreatic cancer cells. When they blocked CD24, there was little effect on pancreatic cancer cell engulfment. Even though flow cytometry provided some information, it was never explained why macrophages still identified many pancreatic cancer cells as positive through the ligand Siglec-10, but the cancer cells did not have enough CD24 to elicit a response. There must be some other glycoprotein utilized as the principal sugar-coated messenger.
Then the scientists used a proximity labeling strategy to discover which specific proteins on pancreatic cells sit next to Siglec-10. From more than 4,000 potential proteins, only a few were promising. However, one pair of proteins in particular stood out. ITGA3 and ITGB1 proteins come together to form the integrin α3β1 complex.
Subsequent evaluations demonstrated that α3β1 exhibits a robust bond with Siglec-10, and this interaction specifically occurs in the presence of sialic acids. The depletion of sialic acid by an enzyme eliminated the interaction of Siglec-10 with α3β1. These insights unveiled a novel "do not eat me" signal that had not been previously acknowledged in pancreatic cancer.
The Implications of This Discovery for Patient Survival
The next step was to determine whether α3β1 could be detected in authentic tumors. Multiple pancreatic cancer cell lines expressed high levels of both integrin subunits, α3 and β1. Likewise, patient tumor samples revealed significantly elevated levels of α3β1 when compared to normal pancreatic tissue.
Increased levels of α3β1 and β1 were associated with worse survival outcomes, while CD24 did not display this pattern. These results solidified the notion that α3β1 may be a central facet in the capacity of tumors to avoid phagocytosis by macrophages.
When analyzing pancreatic tumor cells with low and high levels of α3β1 and β1, researchers observed clear distinctions in immune-based pathways. Cells expressing higher levels of α3β1 presented gene expression patterns associated with immune evasion. Additionally, when high-integrin-expressing cells were removed from the cancer culture, the remaining cancer cells were significantly more susceptible to being engulfed by macrophages.
Antibodies That Release the Immune System’s Restraints
Understanding that tumors are able to use α3β1 to silence Siglec-10 led the research team to a different idea; instead of blocking the interaction between each sugar-coated protein, they aimed to block Siglec-10 itself.
In order to accomplish this, the team immunized mice with human Siglec-10. The team then screened thousands of antibody-producing hybridoma cells until they were able to identify several candidates. One antibody, named 68A11A1, exhibited the highest binding capacity and exhibited the superior function of restoring cancer-eating action in macrophages.
Upon introduction of this antibody to human macrophages and multiple pancreatic cancer lines, macrophages became much more active, engulfing cancer cells at a higher rate than those treated with a CD24-blocking antibody.
Success in Mouse Models Offers Hope
The final experiment was carried out in unique immune-deficient mice implanted with human pancreatic cancer cells. Each mouse was given human macrophages treated with either the Siglec-10 antibody or a control cohort. Tumors in the antibody cohort developed much more slowly.
Macrophages isolated from these treated mice exhibited strong gene expression changes. Genes that enhance immune signaling, motility, and phagocytosis exhibited increased expression, while others that inhibit immune activity decreased. Macrophages also shifted their metabolism to fatty acid utilization, which may serve as an energy source in facilitating sustained immune activation.
The results indicate that blocking Siglec-10 not only disengages the brake but also drives macrophages into a more energized and more durable state consistent with the prevention of pancreatic tumor progression.
A Path Toward Future Treatments
The work illustrates an overlooked sugar-mediated immune escape pathway, in addition to demonstrating that monoclonal antibodies can manipulate that pathway and enhance the defense mechanisms of our bodies. While the mouse studies utilized a more simplistic version of the human immune system, the data represent early efforts towards clinical testing in humans.
Senior author Mohamed Abdel-Mohsen, Northwestern University Feinberg School of Medicine, reflected on this long road to discovery, “It took our team about six years to uncover this novel mechanism, develop the right antibodies and test them,” he said, “It was very exciting to see the discovery work.”
He is optimistic that the new antibody may elicit a synergistic effect with chemotherapy and immunotherapy. “There is a strong scientific rationale to believe that combination therapy will ultimately allow us to achieve our goal, complete remission," he said.
Research findings are available online in the journal Cancer Research.
Related Stories
- Natural sweetener Stevia found safe and effective at killing pancreatic cancer cells
- New synthetic molecule targets and kills breast and pancreatic cancers in as few as three doses
- Breakthrough mRNA vaccine reinvents pancreatic cancer treatment
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joseph Shavit
Writer, Editor-At-Large and Publisher
Joseph Shavit, based in Los Angeles, is a seasoned science journalist, editor and co-founder of The Brighter Side of News, where he transforms complex discoveries into clear, engaging stories for general readers. With vast experience at major media groups like Times Mirror and Tribune, he writes with both authority and curiosity. His writing focuses on space science, planetary science, quantum mechanics, geology. Known for linking breakthroughs to real-world markets, he highlights how research transitions into products and industries that shape daily life.