3D printed living skin and hair follicles revolutionize reconstructive surgery and hair loss treatment
Researchers have found that fat tissue could hold the key to 3D printing layered living skin and potentially hair follicles
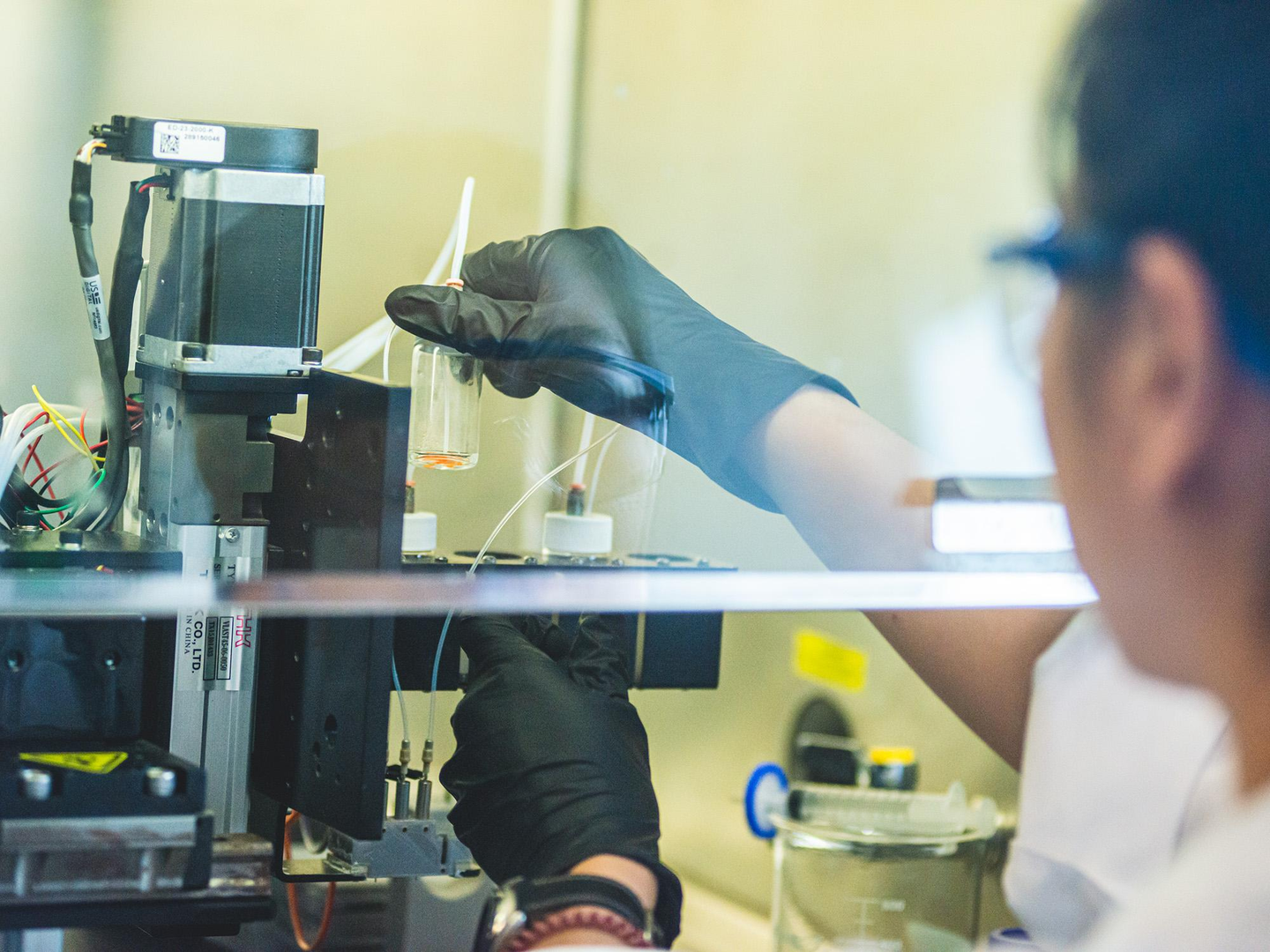
Miji Yeo, a postdoctoral researcher at Penn State, checks the bioink cartridges on a 3D printer developed to intraoperatively print layers of skin. (CREDIT: Michelle Bixby / Penn State)
Researchers have found that fat tissue could hold the key to 3D printing layered living skin and potentially hair follicles, offering new possibilities for reconstructive facial surgery and hair growth treatments.
Led by Ibrahim T. Ozbolat, a professor at Penn State specializing in engineering science, biomedical engineering, and neurosurgery, the team used fat cells and supporting structures from human tissue to repair injuries in rats with remarkable precision.
Their breakthrough, detailed in a recent publication in Bioactive Materials, has earned them a patent for the bioprinting technology they developed. Ozbolat emphasized the significance of their work, stating, “With this work, we demonstrate bioprinted, full thickness skin with the potential to grow hair in rats. That’s a step closer to being able to achieve more natural-looking and aesthetically pleasing head and face reconstruction in humans.”
Histological images of the reconstructed skin stained for H&E (Epi: epidermis layer; Der: dermis layer), MTS (orange arrows indicate blood vessels), LipidTox at Day 14. (CREDIT: Science Direct)
While previous studies have managed to 3D bioprint thin layers of skin, Ozbolat and his team are the first to successfully print a complete, living system of multiple skin layers, including the hypodermis, during surgery. This approach offers the potential for immediate and seamless repair of damaged skin.
The hypodermis, comprised of connective tissue and fat, serves as a crucial support structure over the skull and is directly involved in processes such as wound healing and hair follicle generation.
According to Ozbolat, “The hypodermis is directly involved in the process by which stem cells become fat. This process is critical to several vital processes, including wound healing. It also has a role in hair follicle cycling, specifically in facilitating hair growth.”
Related Stories:
The research began with adipose tissue obtained from patients undergoing surgery at Penn State Health Milton S. Hershey Medical Center. Collaborating with Dino J. Ravnic, an associate professor of surgery at Penn State College of Medicine, the team extracted extracellular matrix from the fat tissue, which provides structure and stability to the tissue, to create one component of the bioink.
Stem cells, harvested from the adipose tissue, were used to create another bioink component. These components were loaded into a bioprinter along with a clotting solution to facilitate proper binding onto the injured site.
“We printed directly into the injury site with the target of forming the hypodermis, which helps with wound healing, hair follicle generation, temperature regulation, and more,” explained Ozbolat.
Graphical abstract: Researchers demonstrated the reconstruction of CMF full-thickness skin defects using intraoperative bioprinting. (CREDIT: Science Direct)
Through a series of studies in rats, the researchers found that the co-delivery of the matrix and stem cells was crucial to hypodermal formation. Additionally, they observed downgrowths in the hypodermis, indicating early hair follicle formation. While fat cells do not directly contribute to the cellular structure of hair follicles, they play a role in their regulation and maintenance.
Ozbolat stated, “In our experiments, the fat cells may have altered the extracellular matrix to be more supportive for downgrowth formation. We are working to advance this, to mature the hair follicles with controlled density, directionality, and growth.”
Intraoperative bioprinting (IOB) for full-thickness skin reconstruction. General schematic of the IOB process using droplet-based bioprinting to reconstruct hypodermis and dermis compartments in a surgical setting. (CREDIT: Science Direct)
The ability to precisely grow hair in injured or diseased sites could significantly enhance the natural appearance of reconstructive surgery outcomes. Ozbolat sees this as a promising development, particularly when combined with other projects from his lab focused on printing bone and matching pigmentation across various skin tones.
“We believe this could be applied in dermatology, hair transplants, and plastic and reconstructive surgeries — it could result in a far more aesthetic outcome,” he remarked.
Looking ahead, Ozbolat envisions the clinical translation of precisely reconstructed skin using fully automated bioprinting technology and compatible materials. This advancement holds the potential to revolutionize the field of reconstructive surgery and offer new hope to patients seeking natural-looking outcomes.
Ravnic and Ozbolat also are affiliated with the Huck Institutes of the Life Sciences and the Penn State Cancer Institute. Ozbolat has additional affiliations with the Penn State Materials Research Institute and the Department of Medical Oncology at Cukurova University in Turkey, where he is currently on sabbatical leave. Other contributors include Yogendra Pratap Singh, postdoctoral scholar, and Mecit Altan Alioglu, graduate student, both in the Penn State Department of Engineering Science and Mechanics; Youngnam Kang and Miji Yeo, both researchers, and Irem Deniz Derman, graduate student, in the Huck Institutes of the Life Sciences; Yang Wu, Harbin Institute of Technology in China; and Jasson Makkar and Ryan R. Driskell, College of Veterinary Medicine at Washington State University. Kang, Yeo, Singh, Alioglu and Derman also are affiliated with Penn State Department of Engineering Science and Mechanics.
The National Institutes of Health and the Scientific and Technological Research Council of Türkiye supported this work.
For more science and technology stories check out our New Innovations section at The Brighter Side of News.
Note: Materials provided above by the The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.