Researchers harness AI and Robotics to treat spinal cord injuries
This study represents one of the first times AI and robotics have been used to formulate highly sensitive therapeutic proteins.
[Mar 8, 2022: Emily Everson Layden, Rutgers University]
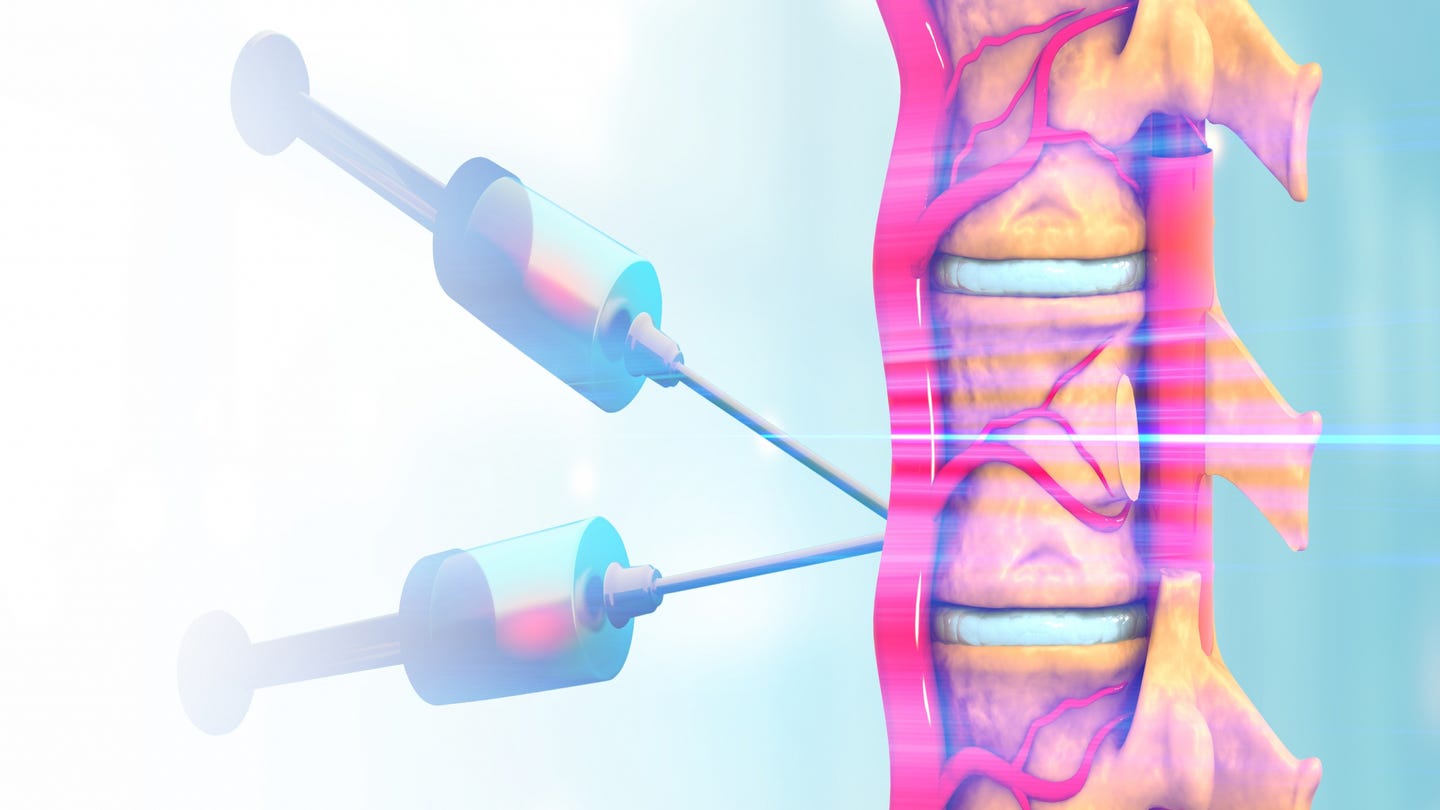
Rutgers researchers are harnessing AI and robotics to deliver new hope for spinal cord injury patients, successfully stabilizing an enzyme able to degrade scar tissue resulting from spinal cord injuries and promote tissue regeneration. (CREDIT: Shutterstock Images)
By employing artificial intelligence (AI) and robotics to formulate therapeutic proteins, a team led by Rutgers researchers has successfully stabilized an enzyme able to degrade scar tissue resulting from spinal cord injuries and promote tissue regeneration.
The study, recently published in Advanced Healthcare Materials, details the team’s ground-breaking stabilization of the enzyme Chondroitinase ABC, (ChABC) offering new hope for patients coping with spinal cord injuries.
“This study represents one of the first times artificial intelligence and robotics have been used to formulate highly sensitive therapeutic proteins and extend their activity by such a large amount. It’s a major scientific achievement,” said Adam Gormley, the project’s principal investigator and an assistant professor of biomedical engineering at Rutgers School of Engineering (SOE) at Rutgers University-New Brunswick.
Gormley expressed that his research is also motivated, in part, by a personal connection to spinal cord injury.
“I’ll never forget being at the hospital and learning a close college friend would likely never walk again after being paralyzed from the waist down after a mountain biking accident,” Gormley recalled. “The therapy we are developing may someday help people such as my friend lessen the scar on their spinal cords and regain function. This is a great reason to wake up in the morning and fight to further the science and potential therapy.”
Related Stories:
Shashank Kosuri, a biomedical engineering doctoral student at Rutgers SOE and a lead author of the study noted that spinal cord injuries, or SCIs, can negatively impact the physical, psychological, and socio-economic well-being of patients and their families. Soon after an SCI, a secondary cascade of inflammation produces a dense scar tissue that can inhibit or prevent nervous tissue regeneration.
The enzyme successfully stabilized in the study, ChABC, is known to degrade scar tissue molecules and promote tissue regeneration, yet it is highly unstable at the human body temperature of 98.6° F. and loses all activity within a few hours. Kosuri noted that this necessitates multiple, expensive infusions at very high doses to maintain therapeutic efficacy.
Synthetic copolymers are able to wrap around enzymes such as ChABC and stabilize them in hostile microenvironments. In order to stabilize the enzyme, the researchers utilized an AI-driven approach with liquid handling robotics to synthesize and test the ability of numerous copolymers to stabilize ChABC and maintain its activity at 98.6° F.
Rutgers researchers harnessed AI and robotics to deliver new hope for patients with spinal cord injuries. (CREDIT: Photo courtesy of Rutgers School of Engineering)
While the researchers were able to identify several copolymers that performed well, Kosuri reported that one copolymer combination even continued to retain 30% of the enzyme for up to one week, a promising result for patients seeking care for spinal cord injuries.
The study received support from grants funded by the National Institutes of Health, the National Science Foundation, and The New Jersey Commission on Spinal Cord research. In addition to Gormley and Kosuri, the Rutgers research team also included SOE Professor Li Cai and Distinguished Professor Martin Yarmush, as well as several SOE-affiliated students. Faculty and students from Princeton University’s Department of Chemical and Biological Engineering also collaborated on the project.
To learn more about the School of Engineering at Rutgers University-New Brunswick, click here.
Two different memory tests designed to study this theory were used. In the first, the participants were shown a series of still images and were asked whether they were from a scene in the film clips they just watched. Study participants were more likely to remember images that occurred soon after a hard or soft boundary, which is when a new “photo” or “event” would have been created.
The second test involved showing pairs of images taken from film clips that they had just watched. The participants were then asked which of the two images had appeared first. It turned out that they had a much harder time choosing the correct image if the two occurred on different sides of a hard boundary, possibly because they had been placed in different “events.”
These findings provide a look into how the human brain creates, stores, and accesses memories. Because event segmentation is a process that can be affected in people living with memory disorders, these insights could be applied to the development of new therapies.
In the future, Dr. Rutishauser and his team plan to look at two possible avenues to develop therapies related to these findings. First, neurons that use the chemical dopamine, which are most-known for their role in reward mechanisms, may be activated by boundary and event cells, suggesting a possible target to help strengthen the formation of memories.
Second, one of the brain’s normal internal rhythms, known as the theta rhythm, has been connected to learning and memory. If event cells fired in time with that rhythm, the participants had an easier time remembering the order of the images that they were shown. Because deep brain stimulation can affect theta rhythms, this could be another avenue for treating patients with certain memory disorders.
This project was made possible by a multi-institutional consortium through the NIH BRAIN Initiative’s Research on Humans program. Institutions involved in this study were Cedars-Sinai Medical Center, Children’s Hospital Boston (site PI Gabriel Kreiman, Ph.D.), and Toronto Western Hospital (site PI Taufik Valiante, M.D., Ph.D.). The study was funded by the NIH BRAIN Initiative (NS103792, NS117839), the National Science Foundation, and Brain Canada.
Note: Materials provided above by Rutgers University. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.
Tags: #New_Discoveries, #New_Innovations, #Medical_News, #AI, #Science, #Spine, #Robotics, #Research, #Technology, #The_Brighter_Side_of_News