Scientists combine magnetic microrobots with ultrasound stimulation to grow new neurons
Disorders like Parkinson’s and Alzheimer’s gradually destroy brain cells, leaving people with worsening memory, movement problems, and few treatment options.

Magnetic cellbots and ultrasound stimulation offer a breakthrough approach to brain regeneration, boosting stem cell therapy precision and success. (CREDIT: Shutterstock)
Neurodegenerative diseases remain some of the most difficult conditions to treat. Disorders like Parkinson’s and Alzheimer’s gradually destroy brain cells, leaving people with worsening memory, movement problems, and few treatment options. Current therapies mostly ease symptoms, but they cannot restore the brain’s lost wiring. That is why scientists have placed such high hopes on stem cell research, a field that could one day help rebuild damaged brain circuits.
Stem cells, unlike specialized cells in the body, have the ability to transform into many different types of cells, including neurons. For brain repair, this flexibility is a crucial advantage. Yet for years, two persistent challenges have slowed progress: delivering stem cells exactly where they are needed and ensuring that those cells reliably develop into functional neurons once they arrive.
A recent study has offered a promising solution by pairing two technologies that, until now, were rarely considered together. The research team combined magnetic microrobots with ultrasound stimulation to guide stem cells to precise locations and encourage their growth into neurons.
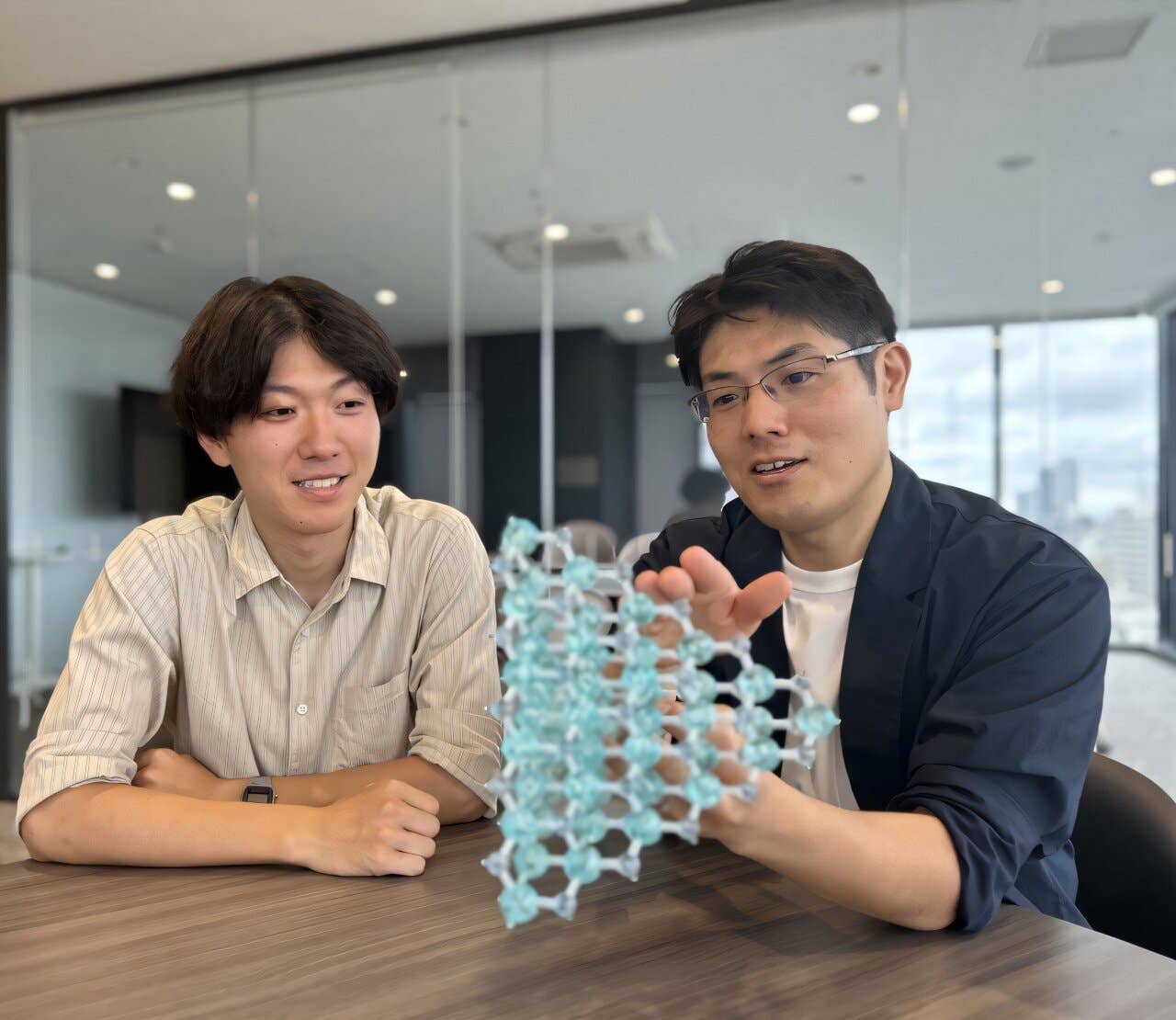
Published in Microsystems & Nanoengineering, the study was led by scientists at the Daegu Gyeongbuk Institute of Science and Technology (DGIST). Their approach has the potential to reshape treatments for neurodegenerative diseases by overcoming long-standing obstacles in stem cell therapy.
Overcoming Barriers in Stem Cell Therapy
Stem cell therapy has long been viewed as a way to replace neurons lost to injury or disease. In practice, however, the process is far from straightforward. Transplanted stem cells often fail to reach their target regions, and even when they do, many remain in an undifferentiated state. This leads to poor integration with existing brain tissue and limited recovery benefits.
Conventional methods to deliver cells, such as surgical injection, carry risks of tissue damage and uneven placement. Magnetic guidance, where stem cells are loaded with iron-based nanoparticles and steered using magnetic fields, improves precision but does not address how to trigger proper neuronal differentiation.
On the other side, ultrasound stimulation has been recognized for its deep tissue penetration and safety. It can influence how cells behave, but standard ultrasound systems lack the fine resolution needed for precise neural engineering.
Related Stories
- New brain map reveals neuron connections behind motor function
- Lab-grown neurons developed to behave exactly like natural ones
The DGIST team realized that by merging these two strategies, they could achieve both goals at once: move cells accurately to damaged brain regions and then stimulate them to become neurons in place.
The Role of Cellbots and pMUTs
The foundation of the system is the use of magnetically responsive microrobots, called Cellbots. These tiny carriers are stem cells loaded with superparamagnetic iron oxide nanoparticles, which allow them to be guided by external electromagnetic fields. In the study, the Cellbots reached target areas at speeds of nearly 37 micrometers per second when exposed to a rotating magnetic field of 20 millitesla. Importantly, this magnetic navigation did not harm the health of the cells.
Once delivered, the second component comes into play: a piezoelectric micromachined ultrasound transducer, or pMUT array. Unlike traditional ultrasound devices, pMUTs are extremely small, with elements just 60 micrometers across. This miniaturized design allows them to focus sound waves with remarkable precision.
The researchers activated different channels of the pMUT sequentially, which prevented overlapping signals and improved the accuracy of stimulation. The device generated acoustic pressures as high as 566 kilopascals, enough to stimulate cells without damaging them. Tests confirmed that the ultrasound pulses were biocompatible, leaving cell viability intact.
Evidence of Enhanced Differentiation
To measure whether the approach truly improved neural differentiation, the scientists tracked neurite outgrowth. Neurites are the thin extensions that grow from neurons and later form synaptic connections. Their length is widely used as a marker of how well stem cells are maturing into functioning neurons.
Results showed a striking improvement. Cells exposed to localized ultrasound after magnetic delivery developed neurites nearly twice as long as those in unstimulated control groups (119.9 ± 34.3 micrometers compared to 63.2 ± 17.3 micrometers). Overall, the system boosted neurite length by around 90%.
This effect confirmed that the cells reached the right place and received the right cues to form networks. The study showed that combining precise delivery with targeted stimulation builds neural connections that neither approach could achieve alone.
Toward New Therapies for Brain Disorders
Dr. Hongsoo Choi, corresponding author, stressed the promise of the integrated method. He said, “Our technology merges the precision of magnetic actuation with the non-invasive power of ultrasound. This creates a scalable platform for neural regeneration. By achieving localized differentiation, we can now envision therapies where stem cells reach their targets and mature into functional neurons on demand.”
The implications extend to many fields. In clinical medicine, the strategy may one day support minimally invasive procedures to treat neurodegenerative diseases. For patients with Parkinson’s or Alzheimer’s, where neuron populations vanish, targeted regeneration could help restore memory or motor functions. Stroke recovery, which depends on reconnecting brain circuits, could also benefit.
In research labs, the method may let scientists build accurate neural tissue models for drug testing. This could reduce reliance on animal studies and accelerate drug discovery. By fine-tuning ultrasound parameters, scientists may also engineer complex networks in culture dishes that mimic human brain activity.
Remaining Challenges and Future Directions
The findings are groundbreaking, but challenges remain before clinical use. One major challenge is ensuring transplanted cells survive and integrate long-term within living brain tissue. Lab results show enhanced differentiation, but maintaining benefits for years in patients remains difficult.
Scaling the system for human use also poses difficulties. Guiding stem cells with magnetic fields in a small lab is easier than in the human brain. Ultrasound delivery requires careful adjustments to avoid heating tissues or causing unwanted effects.
Despite these obstacles, the research represents an important step forward. By uniting magnetic guidance and miniaturized ultrasound stimulation, the team created a new blueprint for stem cell engineering.
A Leap Forward in Neural Engineering
Directing stem cells precisely and stimulating them to become neurons is a long-sought goal in regenerative medicine. The DGIST study shows that this goal is closer than ever. As techniques mature, the approach may reduce invasive surgeries, improve safety, and deliver more reliable outcomes.
Neurodegenerative diseases remain daunting, but breakthroughs like this suggest lost brain connections could be rebuilt. The combination of microrobotics and precision ultrasound may become a cornerstone of future therapies. This progress could reshape how doctors and researchers approach brain repair.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.