Scientists create smart lactation pad to monitor breast milk in real time
A new USC smart pad lets parents check breast milk for acetaminophen in real time, improving infant health and peace of mind.

USC researchers have developed a smart lactation pad that monitors acetaminophen in breast milk, giving parents real-time safety data. (CREDIT: CC BY-SA 4.0)
Breast milk is widely recognized as the gold standard for infant nutrition. It supplies the perfect balance of fats, proteins, and sugars while also delivering antibodies that help newborns fight off infections. The World Health Organization recommends exclusive breastfeeding for the first six months of life due to its many health benefits. But when new mothers are prescribed medications like acetaminophen to manage pain, safety concerns arise.
That's why scientists at the University of Southern California (USC) have built something extraordinary: a smart lactation pad that can test breast milk for medication levels in real time. Their paper, A Wearable Electrochemical Sensor for Monitoring Acetaminophen in Breast Milk, was published in Device. The tool is wearable, disposable, and gives parents peace of mind by analyzing milk without sending it to a lab.
The Risks of Acetaminophen Exposure
Acetaminophen is one of the most commonly prescribed drugs for postpartum pain and for infants with fevers. It's also available over the counter under brand names like Tylenol. Though it’s safe at normal doses, acetaminophen overuse is the leading cause of acute liver failure in children and a top reason for liver transplants in the United States.
Dr. Maral Mousavi, the paper's lead author and an assistant professor of biomedical engineering at USC, explains, “While it is generally safe at recommended doses, acetaminophen overexposure is a leading cause of acute liver failure in children.”
Because drugs taken by breastfeeding mothers can pass into their milk, there’s a need to monitor the safety of the milk, especially when infants have immature livers. Until now, there have been few reliable ways for mothers to check this at home.
Current options often involve mailing samples to labs with long wait times and expensive fees. Some kits cost hundreds of dollars and still don’t offer real-time feedback. Mousavi says, “We wanted to create a tool that empowers parents with real-time, personalized information rather than leaving them to rely on generalized drug-safety charts or delayed lab testing.”
How the Smart Pad Works
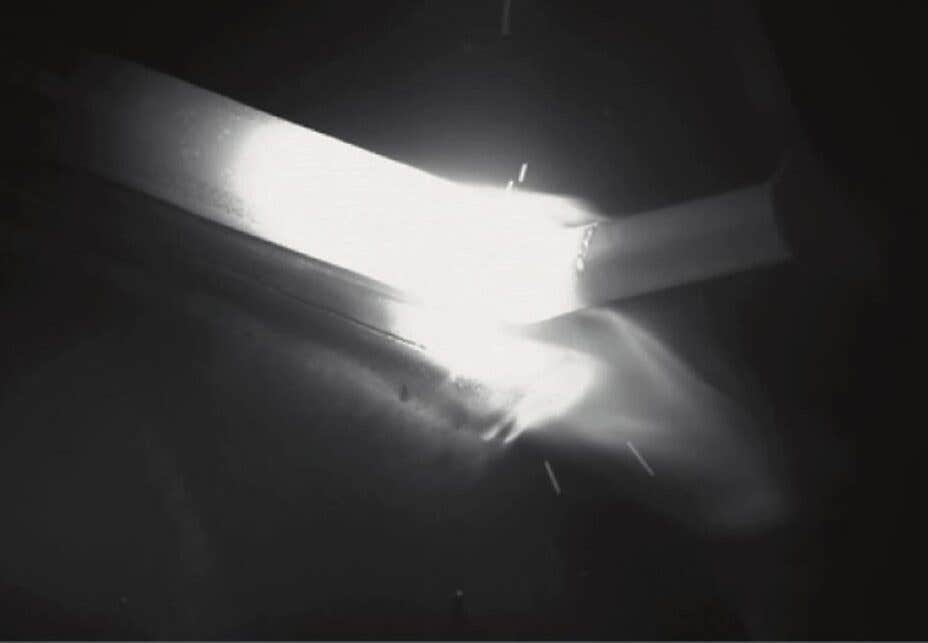
The smart lactation pad looks like a typical nursing pad worn inside a bra to absorb milk leaks. But inside, it's anything but ordinary. It contains microfluidic channels and electrodes made from laser-induced graphene, a material known for its high electrical conductivity.
Related Stories
As breast milk naturally leaks into the pad, a small amount is pulled into the device’s microfluidic channel. There, a special electrode detects acetaminophen by identifying its chemical signature. Within about 30 seconds, data can be read wirelessly by a smartphone app using Bluetooth. This gives the parent a nearly instant snapshot of drug levels in their milk.
The device is based on electrochemical sensing. Acetaminophen molecules undergo oxidation when they meet the electrode's surface. This change produces a measurable signal, allowing the system to calculate drug concentration. Tests showed the system could accurately detect acetaminophen across a wide range of concentrations: from 10 to 600 micromoles per liter.
This kind of measurement is important because different drugs pass into breast milk at different rates, depending on factors like their solubility, size, and how easily they bind to proteins in the blood. The "milk-to-plasma" ratio determines how much of the drug is passed into milk from the bloodstream. Acetaminophen’s ratio varies across people, making personalized testing essential.
Helping Parents Make Informed Choices
A key benefit of the smart pad is helping parents decide when to use the “pump and dump” method. This involves discarding milk produced when drug levels are likely to be high. With the pad, a parent can measure milk right before feeding or pumping to decide if it’s safe.
Mousavi's team was motivated to create this tool when a graduate student in their lab gave birth and was prescribed acetaminophen for pain. Realizing that no convenient tools existed to check milk safety, they designed the smart pad to fill that gap. “This technology has the potential to empower lactating individuals with actionable health insights, supporting both maternal and infant health in ways that have never before been possible,” Mousavi says.
While the current version works best with milk collected from natural leaks, future models are being developed to analyze pumped milk. This will make the tool even more convenient for parents who don’t leak often or prefer to pump.
Beyond painkillers, the pad may soon help detect other drugs like antibiotics or antifungals. Although many of these medications are considered safe during breastfeeding, they are not always risk-free. Another prototype developed by the same USC team can measure glucose in milk, which could help manage conditions like gestational diabetes.
Innovation Behind the Sensor
Creating the smart pad took serious engineering. The sensors were made by laser-engraving polyimide film to create flexible graphene-based electrodes. This process produces carbon structures with a high surface area and excellent electrochemical properties.
The researchers used a method called Central Composite Design (CCD) to fine-tune the sensor’s performance. They tested different combinations of laser power and focal lengths to find the most effective settings. This allowed them to build electrodes that are both accurate and cost-effective.
The paper-based fluid channels inside the pad work through capillary action, pulling milk from the center of the pad to the sensor. A hydrophobic ring prevents contamination by keeping the sensor away from the pad’s absorbent material.
The device's design also allows for continuous or single-point monitoring. Parents can either wear it all day or take a quick test by connecting it to a portable potentiostat. These small, wireless devices collect the data and send it to a smartphone for easy viewing.
Although similar electrochemical sensors have been used to detect acetaminophen in blood, none had been designed for breast milk until now. By combining graphene electrodes, smart circuitry, and user-friendly design, the USC team has developed a tool that could change how mothers manage postpartum recovery.
The Future of Wearable Breast Milk Sensors
This smart lactation pad represents a leap forward in wearable health tech. Unlike fitness trackers or sweat sensors, it directly helps solve a problem unique to postpartum care. Until now, women’s health has been underserved in the wearable tech space. But this breakthrough offers a personalized and science-backed way to support safe breastfeeding.
Mousavi says, “The device opens the door to a new kind of on-body chemical sensing that fits into real life without adding more steps.”
Acetaminophen exposure in infants is a growing concern. The American Academy of Pediatrics advises against giving the drug to children under three months old without medical supervision. Because many cold and flu medicines contain acetaminophen, accidental overdoses can happen when parents aren't aware of all the sources. Each year, over 56,000 emergency room visits in the U.S. are tied to acetaminophen toxicity.
Tools like USC's smart lactation pad could help reduce these numbers by providing accurate, real-time data. Parents will no longer need to guess or rely on outdated charts. Instead, they’ll have evidence-based insights at their fingertips.
While the product is not yet available on the market, the researchers hope their work will lead to new point-of-care technologies that are affordable, accessible, and easy to use. Future versions may offer broader drug detection and smarter integration with apps that guide parents on feeding decisions.
This is more than just a gadget. It’s a move toward greater empowerment in maternal health, giving families tools to care for themselves and their children with confidence.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.