Researchers discover the cause of smell loss from COVID-19
The findings could help to develop treatments for those who are suffering from long-term smell loss following the virus.

[Mar. 30, 2023: Staff Writer, The Brighter Side of News]
Findings provide insight into a vexing problem that has plagued millions who have not fully recovered their sense of smell after COVID-19. (CREDIT: Creative Commons)
Duke Health scientists have identified an ongoing immune assault on olfactory nerve cells as the reason why some COVID-19 patients are unable to recover their sense of smell.
The findings could help to develop treatments for those who are suffering from long-term smell loss following the virus. Furthermore, the results might shed light on the underlying causes of other long COVID-19 symptoms, such as generalized fatigue, shortness of breath, and brain fog.
According to a new study published in the journal Science Translational Medicine, the researchers analyzed olfactory epithelial samples from 24 biopsies, including nine patients experiencing long-term smell loss.
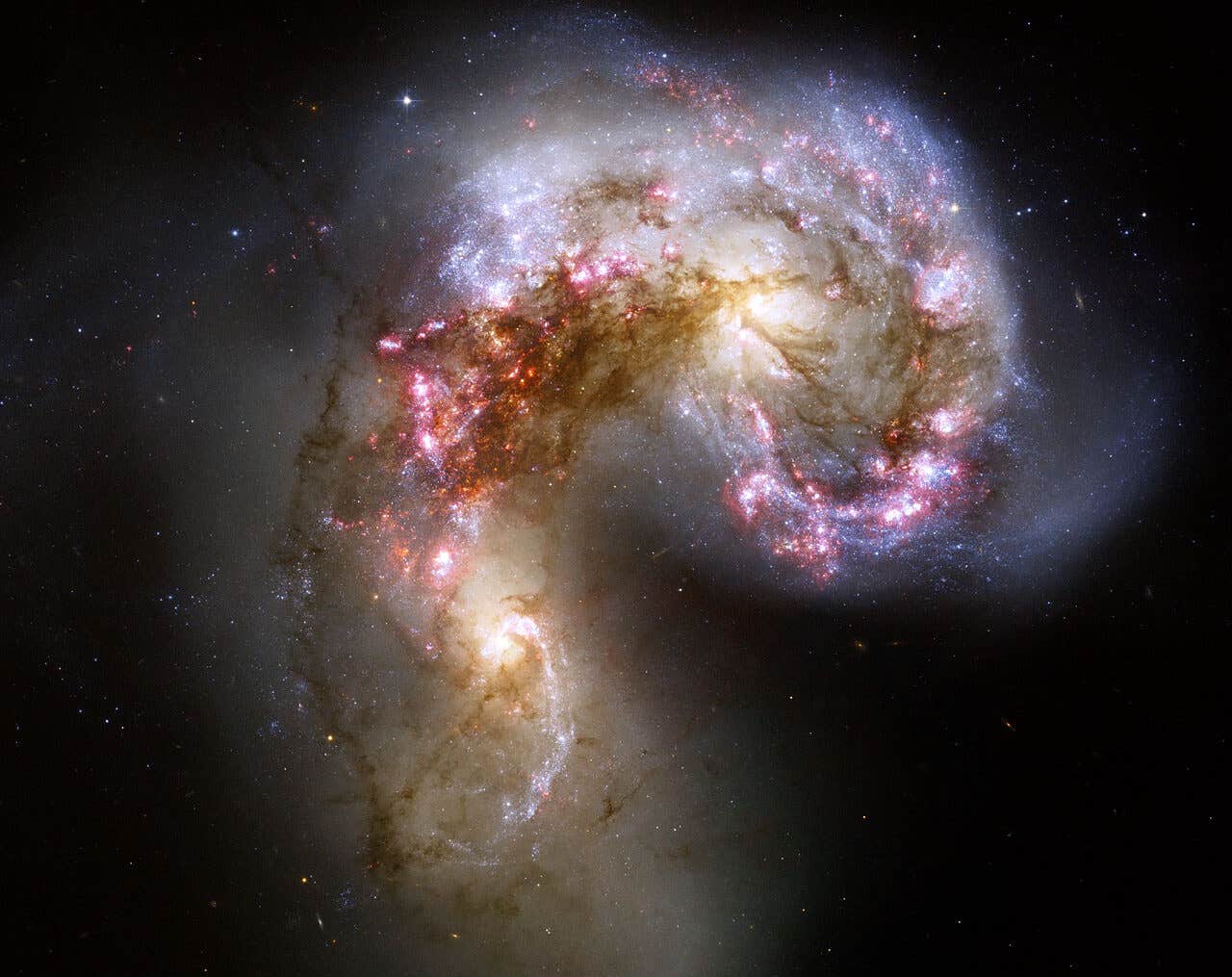
The researchers collaborated with Sandeep Datta, M.D., Ph.D., at Harvard University to utilize a biopsy-based approach, utilizing sophisticated single-cell analyses. They found that patients with long-term smell loss exhibited a widespread infiltration of T-cells that were engaging in an inflammatory response in the olfactory epithelium.
Related Stories:
This process of inflammation persisted despite the absence of detectable SARS-CoV-2 levels. Additionally, the number of olfactory sensory neurons was reduced, which could be due to damage caused by the ongoing inflammation.
“One of the first symptoms that has typically been associated with COVID-19 infection is loss of smell,” said Bradley Goldstein, M.D., Ph.D., the senior author of the study and an associate professor in Duke’s Department of Head and Neck Surgery and Communication Sciences and the Department of Neurobiology.
“Fortunately, many people who have an altered sense of smell during the acute phase of viral infection will recover smell within the next one to two weeks, but some do not. We need to better understand why this subset of people will go on to have persistent smell loss for months to years after being infected with SARS-CoV-2”, Goldstein continued.
T cell infiltrates in nasal olfactory epithelial biopsies from PASC hyposmic patients. (CREDIT: Science Translational Medicine)
Dr. Goldstein said that the findings were significant, as they resemble an autoimmune-like process in the nose. He also mentioned that identifying what sites are damaged and what cell types are involved is a crucial step towards designing treatments.
The researchers were encouraged to find that neurons appeared to maintain some ability to repair themselves, even after the long-term immune onslaught. “We are hopeful that modulating the abnormal immune response or repair processes within the nose of these patients could help to at least partially restore a sense of smell,” Goldstein said, noting that his lab is currently working on this.
A CD8+ T cell subset is enriched in nasal olfactory epithelial biopsies from PASC hyposmic patients. (CREDIT: Science Translational Medicine)
The study’s findings could also help researchers to understand the underlying causes of other long COVID-19 symptoms that might be undergoing similar inflammatory processes. The researchers said that their work highlights the need for more research into long-term effects of COVID-19 and the development of treatments for those suffering from such symptoms.
The COVID-19 pandemic has affected millions of people worldwide, and many patients have reported experiencing long-term symptoms even after their initial infection has cleared. These long-term symptoms are commonly referred to as “long COVID-19” and can include symptoms such as fatigue, brain fog, and shortness of breath. However, one of the most common symptoms reported by patients is a loss of smell.
PASC hyposmic olfactory epithelial biopsies show a myeloid cell shift with enriched DC subsets and decreased M2 macrophages. (CREDIT: Science Translational Medicine)
While many patients recover their sense of smell within a few weeks of infection, some experience persistent smell loss that lasts for months or even years. The new study’s findings provide important insights into the underlying causes of this long-term smell loss and could help to develop treatments for those affected.
The study highlights the need for further research into the long-term effects of COVID-19 and the development of treatments for those suffering from long-term symptoms. The researchers said that their findings could also inform additional research into other long COVID-19 symptoms that might be undergoing similar inflammatory processes.
In addition to Goldstein and Datta, study authors include John B. Finlay, David H. Brann, Ralph Abi-Hachem, David W. Jang, Allison D. Oliva, Tiffany Ko, Rupali Gupta, Sebastian A. Wellford, E. Ashley Moseman, Sophie S. Jang, Carol H. Yan, Hiroaki Matusnami, and Tatsuya Tsukahara.
The study received funding support from the National Institutes of Health (DC018371, DC016859, AG074324, DC019956) and the Duke Department of Head and Neck Surgery & Communication Sciences.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.