Scientists harness bacteria to deliver cancer-killing virus and halt tumor spread
The idea is bold: hide a virus inside a bacterium, smuggle it safely into a tumor, and then unleash it to destroy cancer cells.
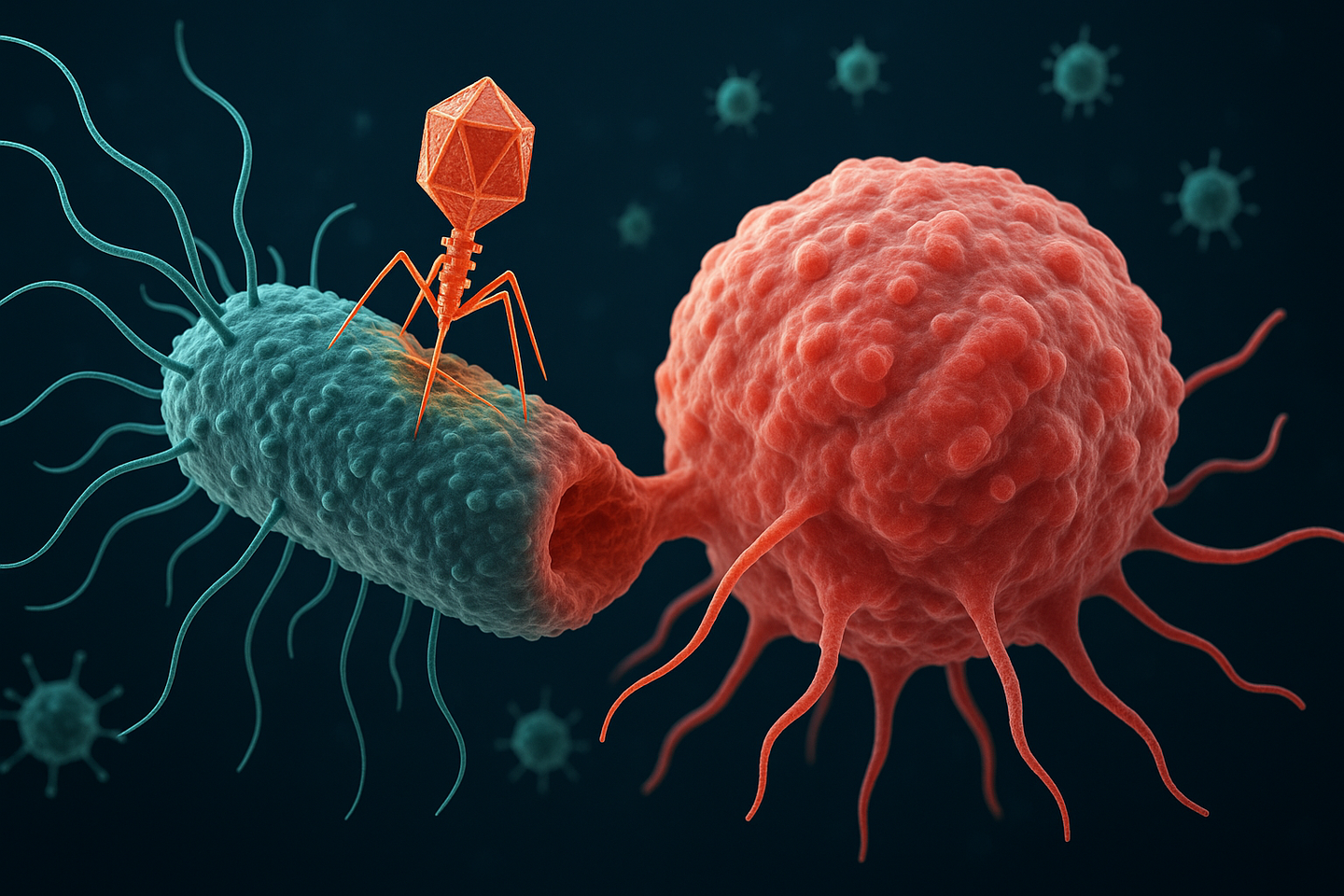
CAPPSID cancer therapy hides a virus inside a bacterium, sneaks past immune defenses, and destroys tumors from within. (CREDIT: AI-Generated / The Brighter Side of News)
Cancer research has long looked at bacteria and viruses as separate tools for therapy. Now, researchers are showing that the two can actually work better together. A team of scientists has built a new system called CAPPSID, short for Coordinated Activity of Prokaryote and Picornavirus for Safe Intracellular Delivery. The idea is bold: hide a virus inside a bacterium, smuggle it safely into a tumor, and then unleash it to destroy cancer cells.
This fresh approach, published in Nature Biomedical Engineering, could change the way you think about cancer treatment. It takes advantage of the natural instincts of microbes while adding layers of engineering to keep the therapy safe.
A Microbial Partnership
The project is led by Tal Danino, an associate professor of biomedical engineering at Columbia University, in collaboration with virologist Charles M. Rice at The Rockefeller University. Their system works by programming Salmonella typhimurium, a bacterium known for homing in on tumors, to carry Senecavirus A, an oncolytic virus. Together, they form a cooperative team with one mission: infiltrate tumors and destroy them from the inside.
Co-lead author Jonathan Pabón, an MD/PhD candidate at Columbia, explained the motivation. “We aimed to enhance bacterial cancer therapy by enabling the bacteria to deliver and activate a therapeutic virus directly inside tumor cells, while engineering safeguards to limit viral spread outside the tumor.”
You might wonder why anyone would hide a virus inside a bacterium in the first place. The answer lies in your immune system. Oncolytic viruses are designed to infect and kill cancer cells, but if your body already has antibodies against them, the immune system neutralizes the virus before it can act. That’s where the bacteria come in.
“The bacteria act as an invisibility cloak, hiding the virus from circulating antibodies, and ferrying the virus to where it is needed,” says Zakary S. Singer, co-lead author and former postdoctoral researcher in Danino’s lab.
Related Stories
- Study finds surprising links between regular exercise, your liver and brain health
- New machine learning program accurately predicts who will stick with their exercise program
Sneaking Past Immune Defenses
One of the toughest challenges in cancer virotherapy is the immune response. Your body is skilled at detecting and fighting viruses, especially those you’ve already encountered through infection or vaccination. That immune memory can block a therapeutic virus before it ever reaches a tumor.
By using bacteria as carriers, the Columbia team found a clever workaround. The virus remains hidden inside its bacterial partner until it arrives at its target. Once inside the tumor, the bacterium delivers the viral RNA, effectively planting the seeds of infection in the cancer cells.
“Our system demonstrates that bacteria can potentially be used to launch an oncolytic virus to treat solid tumors in patients who have developed immunity to these viruses,” Pabón says.
How CAPPSID Targets Tumors
The bacterial side of the system relies on the natural instincts of Salmonella typhimurium. These bacteria thrive in the nutrient-rich, low-oxygen environment inside tumors. Once they invade, they break open and release the virus directly into cancer cells.
“We programmed the bacteria to act as a Trojan horse by shuttling the viral RNA into tumors and then lyse themselves directly inside of cancer cells to release the viral genome, which could then spread between cancer cells,” Singer explains.
This Trojan horse strategy allows the virus to spread throughout the tumor, overcoming one of the biggest limitations in single-microbe therapies. Viruses alone often fail to reach enough tumor cells, while bacteria alone typically remain trapped inside the tumor core. Together, they achieve what neither could do alone.
“This is probably our most technically advanced and novel platform to date,” Danino says.
Building in Safety Controls
A major concern with live-virus therapy is preventing the infection from escaping into healthy tissue. The CAPPSID system addresses this by engineering dependence between the virus and the bacteria. The virus cannot complete its life cycle without a bacterial enzyme, a protease, that is only present where the bacteria are active.
“Spreadable viral particles could only form in the vicinity of bacteria, which are needed to provide special machinery essential for viral maturation in the engineered virus, providing a synthetic dependence between microbes,” Singer says.
That safeguard ensures that even if viral particles drift beyond the tumor, they won’t be able to multiply in normal tissues.
“It is systems like these — specifically oriented towards enhancing the safety of these living therapies — that will be essential for translating these advances into the clinic,” Singer adds.
Toward Clinical Translation
The research team has already filed a patent application (WO2024254419A2) with the U.S. Patent and Trademark Office for this technology. The next step is to test the approach in more cancer types and different models. They also want to build a broader “toolkit” of viruses that can sense and respond to the unique conditions inside a cell.
“As a physician-scientist, my goal is to bring living medicines into the clinic,” Pabón says. “Efforts toward clinical translation are currently underway to translate our technology out of the lab.”
Researchers are also exploring how this system might be combined with strains of bacteria that have already been shown to be safe in human trials. That step could speed the path toward real-world treatments.
Beyond One Microbe
The idea of mixing microbes might sound new, but nature has been doing it for a long time. In natural co-infections, bacteria and viruses often interact directly. Sometimes they even bind to one another, enhancing their ability to survive.
Synthetic biology is now catching up to these natural partnerships. By designing cooperation between bacteria and viruses, researchers are opening the door to more sophisticated therapies. CAPPSID may be the first direct example of such engineered cooperation against cancer.
This cooperative model also mirrors the diversity of microbes themselves. Different bacteria are suited for different jobs: Staphylococcus epidermidis thrives on skin, Mycoplasma pneumoniae targets lungs, Listeria monocytogenes grows inside cells, and Salmonella typhimurium homes in on tumors. Viruses are equally varied, from small DNA viruses like adeno-associated virus, to minus-strand RNA viruses like rabies, to plus-strand RNA viruses like poliovirus derivatives. Each has unique features that make it useful for therapy.
By combining these capabilities, scientists can design microbial communities that do what no single microbe can accomplish on its own.
A Glimpse at the Future
Cancer therapies are moving into a new phase where engineered living systems could join the medical toolkit. Instead of relying only on drugs or radiation, future treatments might deploy cooperative microbes designed to target, infiltrate, and dismantle tumors.
“By bridging bacterial engineering with synthetic virology, our goal is to open a path toward multi-organism therapies that can accomplish far more than any single microbe could achieve alone,” Singer says.
If this work moves forward successfully, you may one day see cancer therapies that rely not just on engineered cells, but on whole microbial partnerships. CAPPSID is one of the first steps toward that future.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.