Scientists use light-controlled nanorobots to quickly grow bone cells
Nanorobots and gentle pressure pulses use pure mechanics to turn stem cells into bone builders, pointing to safer future therapies.

 Edited By: Joseph Shavit
Edited By: Joseph Shavit
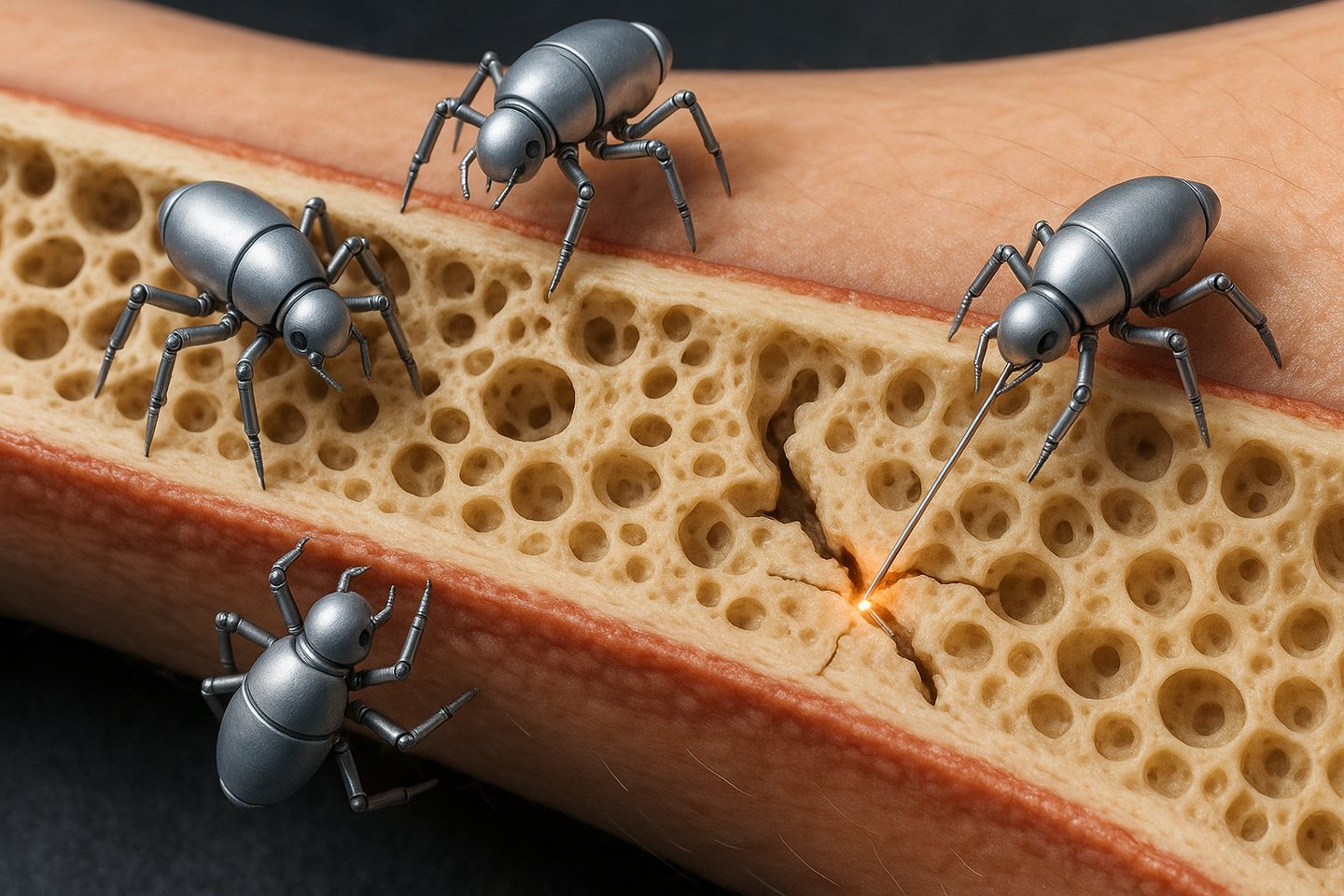
Researchers in Munich and beyond have shown that tiny gold nanorobots and soft microgels under rhythmic pressure can guide stem cells into bone forming cells using only mechanical forces, opening a path toward faster, more natural regenerative treatments. (CREDIT: AI-generated / The Brighter Side of News)
A tiny fleet of gold nanorobots is teaching stem cells how to become bone. At the same time, another lab is using gentle pulses of pressure to coax single cells into building mineral and collagen. Together, these two lines of research point to a future where doctors guide your cells with physics, not just drugs, to repair broken bones and damaged tissue.
Teaching Cells With Gentle Force
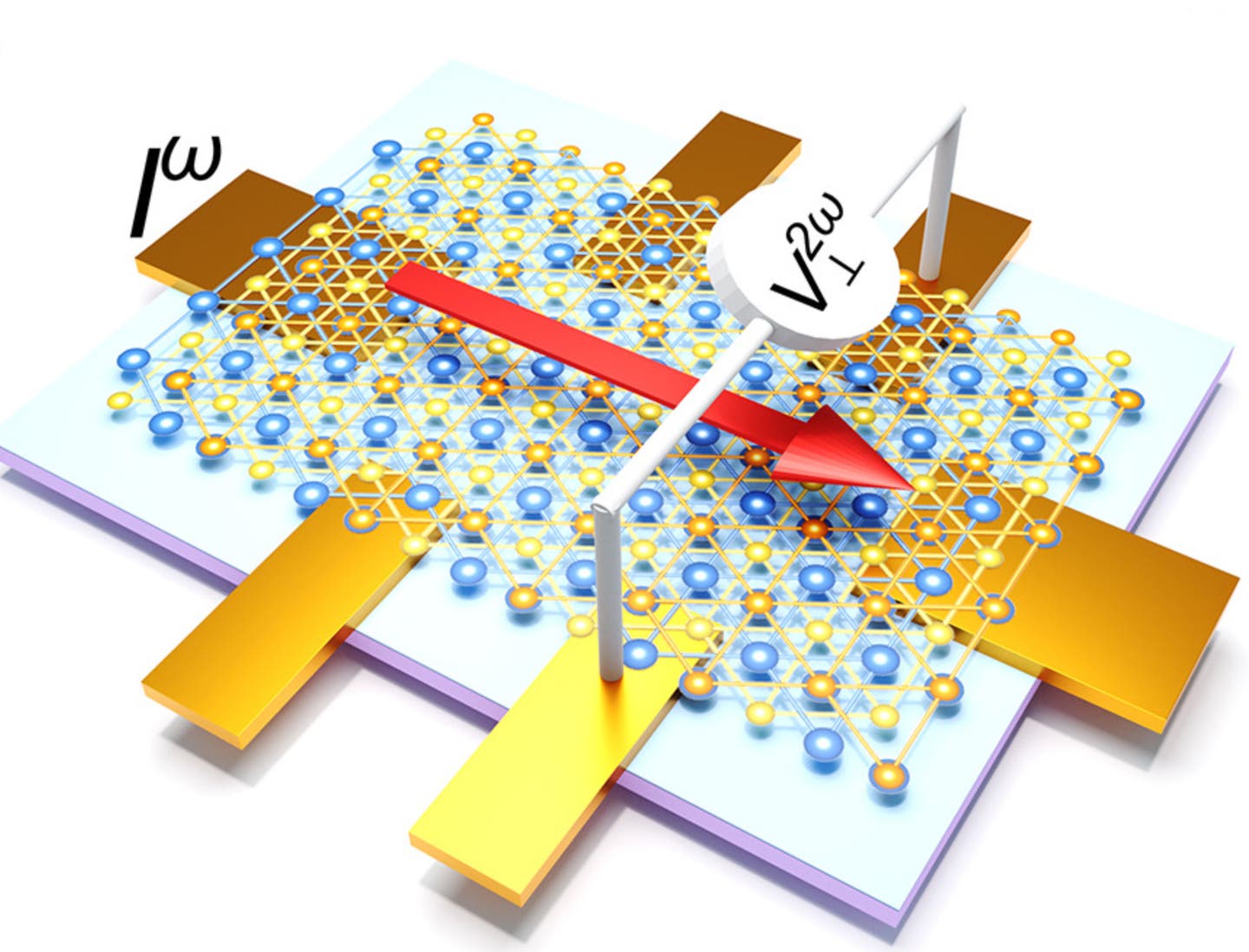
At the Technical University of Munich, Prof. Berna Özkale Edelmann and her team have built nanorobots that look almost playful, yet work with surgical precision. Each robot is a tiny structure made of gold rods and plastic chains. Millions of them sit inside a soft gel cushion only about 60 micrometers across, along with a few human stem cells.
Laser light powers and steers these robots. When the laser heats the gel in a very local spot, the robots press on specific points of the cell membrane with a known force. “We heat the gel locally and use our system to precisely determine the forces with which the nanorobots press on the cell – thereby stimulating it,” explains Özkale Edelmann, professor of nano- and microrobotics at Munich.
That pressure is more than a nudge. It sets off biochemical signals inside the cell. Ion channels open and close differently, and key proteins switch on, including one that plays a central role in bone formation. If the team applies the right rhythm and a low but steady force, a stem cell can be reliably pushed to become a bone cell within three days. The full transformation finishes in about three weeks.
“It’s almost like at the gym: we train the cells for a particular area of application. Now we just have to find out which stress pattern suits each cell type,” says Özkale Edelmann, who leads the Microbiotic Bioengineering Lab at TUM. Her group believes that similar “training plans” can also be found for cartilage cells and heart muscle cells.
From Repair Cells To Bone Builders
The Munich work focuses on mesenchymal stem cells, often called the body’s repair cells. These cells are about 10 to 20 micrometers in size and can turn into bone, cartilage or muscle. They are valuable for regenerative medicine, yet hard to control. In many current therapies, doctors rely on chemical cocktails that do not always give consistent results.
“We have developed a technology that allows forces to be applied to the cell very precisely in a three-dimensional environment,” says Özkale Edelmann. She calls this an unprecedented advance. Instead of bathing cells in growth factors, the team can now talk to each cell through small, measured pushes.
The goal is not only control, but also scale. A real treatment would need at least a million well trained cells, far more than a single gel cushion can hold. “That’s why the next step is to automate our production process so that we can produce more cells more quickly,” Özkale Edelmann explains. The vision is an automated line where many gel pads, each packed with nanorobots and stem cells, run through a precise exercise program and emerge as ready made bone, cartilage or heart cells.
A Second Path: Pressure Pulses in Soft Microgels
In a separate project, another team has shown that force alone can guide stem cells toward bone, even inside very soft materials that could one day be injected into the body. Their system looks very different from the Munich nanorobots, but it speaks the same mechanical language.
These researchers encapsulated single mesenchymal stem cells inside tiny alginate microgels, each about 30 micrometers wide. The gels were coated with extra layers to keep cells from escaping and to hold them for at least three weeks. Cell survival stayed high, around 80 to 90 percent, which means the cells tolerated their small homes well.
The microgels then sat inside sealed plastic tubes filled with culture medium. By using a pressure controller on the air at the top of each tube, the team could deliver rhythmic hydrostatic pressure through the liquid to every microgel at once. Their standard “workout” was simple but strict: 200 kilopascals of pressure at 0.5 hertz, with a 50 percent duty cycle, for 30 minutes per day over 21 days. No chemical osteogenic factors were added.
Under this routine, the cells began to change. A key mechanosensitive protein called YAP moved into the nucleus during the first two weeks, a classic sign that a cell is translating physical cues into gene activity. The master bone transcription factor RUNX2 increased, especially early in the process. Alkaline phosphatase, an enzyme linked to bone matrix preparation, rose over time as well.
By the third week, the cells were producing collagen type I, which makes up most of bone matrix, and laminin, another important signaling protein. Dark, opaque spots appeared in the microgels, marking the first mineral deposits. All of this happened in a material with a stiffness of only about 1 to 2.5 kilopascals, much softer than typical bone forming scaffolds, and without any added biochemical induction medium.
Steering Cells With Physics, Not Only Chemistry
When you place these two studies side by side, a shared message appears. Stem cells listen closely to the forces around them. Whether the signal comes from gold based nanorobots pressing on their membranes or from pressure waves moving through a soft gel, the cells read those mechanical cues and adjust their fate.
For you as a future patient, that may sound distant, but the idea is very personal. If you break a bone or lose tissue after an accident, doctors may one day rebuild what you lost by “training” your own stem cells with physical patterns instead of complex drug mixes. The cells could be guided to form sturdy bone or flexible cartilage that better matches your natural tissue.
These methods might also reduce some safety concerns that come with high dose growth factors or genetic manipulation. Mechanical signals are the same kind of cues your body already uses when you walk, lift, or even breathe. Turning them into precise tools, however, will take more work. Each cell type appears to need its own stress rhythm, its own duration and its own intensity. Scaling both the nanorobot system and the microgel pressure platform to produce millions of cells reliably will also be a major engineering challenge.
Still, both projects suggest a future where your cells are “coached” rather than simply drugged, and where physics becomes a central part of regenerative medicine.
Practical Implications of the Research
These findings show that doctors may eventually steer stem cells with controlled force patterns instead of relying mainly on chemical cocktails. That shift could lead to safer and more natural cell therapies, especially for bone repair, cartilage replacement and heart muscle regeneration.
For patients with fractures, osteoporosis or joint damage, nanorobot trained bone cells or mechanically guided bone forming microgels could shorten healing times and improve the quality of new tissue. Surgeons might one day inject soft, pressure responsive gels into defects, then apply external mechanical cues to help your own cells build new bone from the inside out.
In the lab, these systems offer powerful new test beds. Researchers can study how single stem cells respond to precise 3D forces, map the exact signaling pathways that turn on, and design custom mechanical “training plans” for different lineages. That knowledge will deepen basic understanding of how the body uses physical cues to shape organs during growth and repair.
Finally, automation of nanorobot platforms and scalable pressure chambers could allow factories of personalized cells, where your own stem cells are expanded and mechanically programmed before treatment. That would bring regenerative medicine closer to routine clinical use, with therapies that are faster, more tailored and more closely matched to how your body naturally heals.
Research findings are available online in the journal Small Science.
Related Stories
- Urine-powered nanorobots shrink bladder tumors by 90%, study finds
- World’s smallest battery works in blood to power medical sensors
- Scientists propose simple new way to spot alien life in the universe
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Writer and Editor
Joshua Shavit is a NorCal-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a co-founder of The Brighter Side of News, he focuses on positive and transformative advancements in technology, physics, engineering, robotics, and astronomy. Joshua's work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.