Smart bandage tracks and treats chronic wounds in real time
A smart bandage called iCares tracks infection, inflammation, and healing in real time—offering new hope for chronic wound patients.
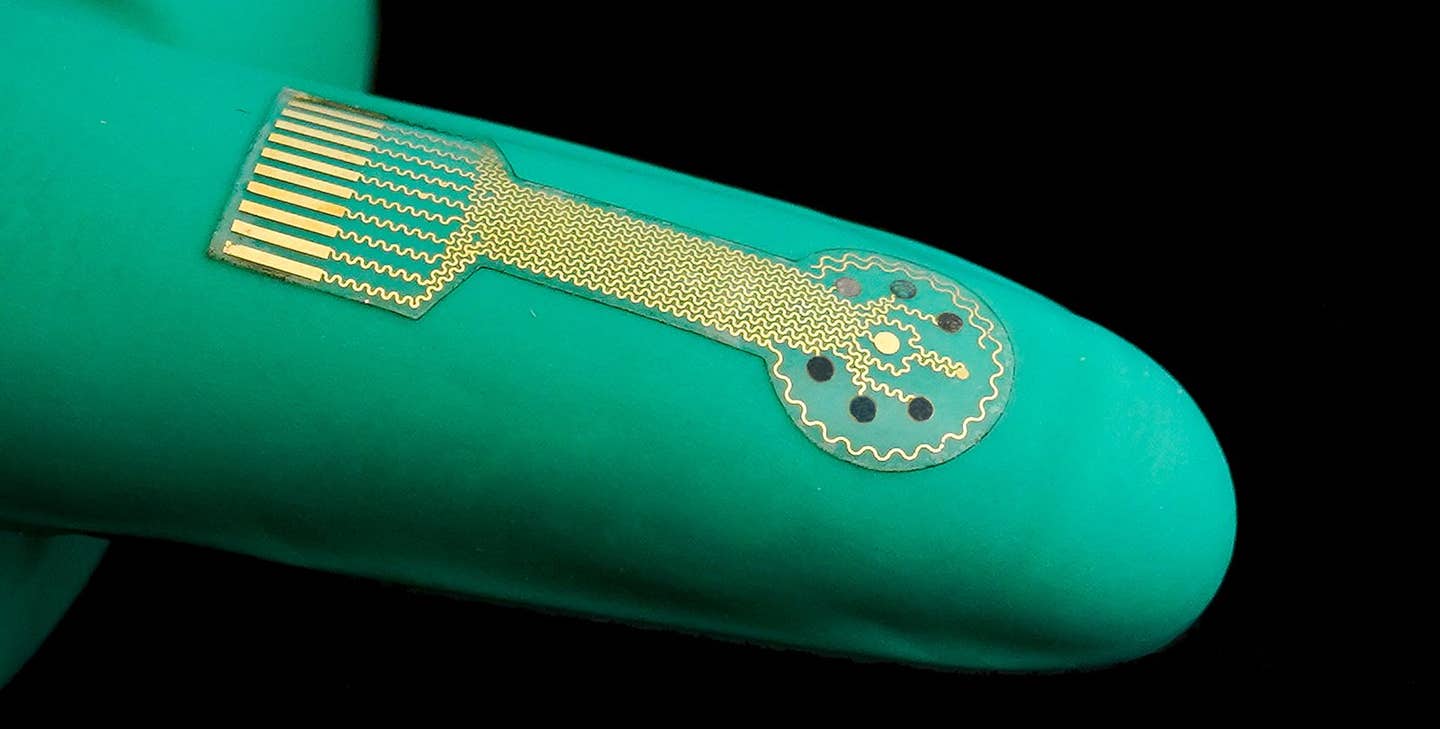
New smart bandage offers real-time monitoring and fluid analysis to speed healing of chronic wounds and prevent infection. (CREDIT: Caltech)
Chronic wounds affect millions of people worldwide. These are cuts, burns, scrapes, or surgical wounds that don’t heal within a normal time. When left untreated or improperly managed, they can cause infection, long-term damage, and emotional distress. People with diabetes or poor circulation are especially at risk.
Treating these wounds is expensive and time-consuming, placing a heavy burden on healthcare systems. But a new smart bandage technology called iCares could soon change how these wounds are treated—and it works right on the skin.
A Smart Bandage That Sees Beneath the Surface
Engineers from Caltech have developed iCares, a wearable smart bandage that does far more than cover a wound. It checks the wound in real time and sends updates to a smartphone or computer. The bandage measures important signs like temperature, pH, and oxygen levels at the wound site. It also detects molecules like nitric oxide (NO) and hydrogen peroxide (H₂O₂), which signal inflammation or infection. These chemical clues, or biomarkers, tell doctors or caregivers what’s going on beneath the surface, even before symptoms appear.
"Our innovative microfluidics remove moisture from the wound, which helps with healing,” says Wei Gao, a medical engineer involved in the project. “They also make sure that samples analyzed by the bandage are fresh, not a mixture of old and new fluid. To get accurate measurements, we need to sample only the newest fluid at a wound site.” The goal is simple: help wounds heal faster and catch problems earlier. But the technology behind it is anything but simple.
Engineering a “Lab on Skin”
The iCares system includes three smart modules that move and analyze wound fluid—also called exudate. These tiny channels collect fresh fluid directly from the wound and guide it toward sensors. One part of the system absorbs fluid using a special membrane that mimics natural materials. Another uses thin wedge-shaped channels that move fluid quickly without pumps. A third part with tiny 3D-printed pillars ensures fluid flows in one direction, keeping things clean and clear.
At the heart of the bandage lies a nanoengineered sensor array. These ultra-small sensors detect chemical changes in the wound fluid, giving doctors an up-to-date look at how the wound is doing. For example, a spike in hydrogen peroxide means an infection may be forming. A drop in oxygen might mean poor blood supply. Tracking these changes in real time allows for more accurate and timely treatment.
Related Stories
This kind of close-up monitoring wasn’t possible before. Most current systems only collect fluid after it's already mixed with older samples, making it harder to read. Plus, they don’t measure multiple markers at once, and they certainly can’t send updates to a phone.
Real-World Testing in People and Mice
This isn't just an idea in a lab. Researchers tested iCares in real patients and in animal models. First, they applied it to diabetic mice with infected skin wounds. The bandage tracked inflammation and infection over time, even during antibiotic treatment. This early testing showed that the sensors stayed accurate and that the system could work continuously for days.
Then, the team tested iCares on 20 human patients with chronic wounds. These wounds weren’t healing on their own due to underlying issues like poor circulation or diabetes. The researchers also used the bandage on two more patients before and after surgery to compare healing progress.
In all cases, the system successfully collected fresh wound fluid, measured biomarkers, and sent data wirelessly. The patients’ wounds showed key changes—like increases in nitric oxide and hydrogen peroxide—one to three days before doctors could see visible signs of infection or inflammation.
To take things even further, the team built a machine learning model. This program looked at the bandage’s sensor data and could classify how bad the wound was and predict how long it would take to heal. Its accuracy matched that of trained clinicians.
Designed for Mass Use and Real-World Impact
One major benefit of iCares is how easy it is to make. The bandage uses flexible, skin-friendly materials that can be 3D printed at low cost. Each sensor array is disposable, keeping things hygienic and safe. The electronic circuit board can be reused and connects to devices like smartphones through wireless signals. These features make iCares both affordable and practical for hospitals, clinics, and even home care.
Gao and his colleagues call it a “lab on skin.” The idea is to give doctors a way to monitor a wound 24/7 without needing expensive lab tests or guesswork. It also lets patients stay active without worrying about taking off bandages or making frequent visits.
The smart bandage doesn’t just report problems—it could one day treat them. In earlier tests, the team used a related device to apply medicine or mild electric currents to the wound to help it heal. Future versions of iCares might include these features too, combining diagnosis and treatment in one simple patch.
Why Monitoring Matters in Chronic Wounds
Chronic wounds are stubborn. They don’t heal quickly because something in the body is holding the process back. It might be low oxygen, slow cell growth, poor blood flow, or a mix of problems. The only way to treat these wounds well is to understand exactly what’s wrong—and when it changes.
That’s where biomarkers come in. Molecules like nitric oxide and hydrogen peroxide can tell doctors if the body is trying to fight infection or if inflammation is too high. High pH levels, low oxygen, and rising temperatures also give clues about the healing process.
But these signs change over time. A single test won’t help. You need a system that watches around the clock. That’s what iCares does best.
A Step Closer to Personalized Care
The big picture goes beyond just one bandage. The iCares system represents a shift in how doctors treat wounds and monitor recovery. By combining smart sensors, wireless data, and machine learning, the technology offers a personalized approach to healing. Every patient’s wound is different, and iCares adapts to those differences in real time.
With this kind of data, caregivers can make better decisions. They can apply antibiotics sooner, adjust treatment plans faster, and avoid infections before they start. Patients feel more in control, and doctors get clearer, faster insights.
The smart bandage still has more testing ahead before it’s used widely. But with this study, researchers have shown that the future of wound care might already be here—and it fits in the palm of your hand.
Research findings are available online in the journal Science Translational Medicine.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.