Ultra-precise human heart map can even pinpoint where heartbeats come from
The Atlas is a leap forward in understanding the intricacies of the human heart, including the specialized tissue of cardiac conduction.
[July 14, 2023: Staff Writer, The Brighter Side of News]
In a ground-breaking discovery that defies conventional medical understanding, three elderly men with heart failure caused by a build-up of sticky, toxic proteins have experienced a reversal of their condition. (CREDIT: Creative Commons)
In a groundbreaking research study, a group of scientists has unveiled the most comprehensive and detailed Human Heart Cell Atlas to date. Published in the renowned scientific journal Nature, the Atlas is a leap forward in understanding the intricacies of the human heart, encompassing even the specialized tissue of the cardiac conduction system, from where the heartbeat originates.
Leading the study was an international multi-center team from the Wellcome Sanger Institute and the National Heart and Lung Institute at Imperial College London. A new computational tool, "Drug2cell," was also introduced, providing valuable insights into the effects of various drugs on heart rate.
"This Heart Cell Atlas reveals cardiac microanatomy in unprecedented detail, including the cardiac conduction system that enables each heartbeat, and is a valuable reference for studying heart disease and designing potential therapeutics," said Dr. Sarah Teichmann, a senior author of the study from the Wellcome Sanger Institute and co-chair of the Human Cell Atlas Organising Committee.
This groundbreaking work forms part of the international Human Cell Atlas (HCA) initiative, an ambitious global effort to map every cell type in the human body. The ultimate goal of this initiative is to revolutionize our understanding of health and disease. The Human Heart Cell Atlas serves as the foundation for a fully integrated HCA Human Heart Cell Atlas.
Related Stories
Astonishingly, the study charts eight distinct regions of the human heart, describing a total of 75 different cell states. These include the cells of the cardiac conduction system, a group of cells responsible for the heartbeat. Their functioning, until now, had not been comprehended at such a granular level in humans before.
The cardiac conduction system, considered the heart's 'wiring,' transmits electrical impulses from the top to the bottom of the heart, coordinating the heartbeat. Utilizing spatial transcriptomics—a technique that provides a “map” of where cells are positioned within a tissue—the researchers gleaned a profound understanding of how these cells communicate with each other for the first time. This map acts as a molecular guidebook, presenting what healthy cells look like, which will be critical to understand the anomalies occurring in diseased states.
"The cardiac conduction system is critical for the regular and coordinated beating of our hearts, yet the cells which make it up are poorly understood. This study sheds new light by defining the profiles of these cells, as well as the multicellular niches they inhabit. This deeper understanding opens the door to better, targeted anti-arrhythmic therapies in the future,” said Dr. James Cranley, a cardiologist specializing in heart rhythm disorders and PhD student at the Wellcome Sanger Institute, who is the joint first author of the study.
Multimodal profiling of the adult human heart. H&E micrographs of the SAN, the AVN and the AVB (yellow bordered). P cells in the nodal tissue (red box) are smaller than neighbouring CMs in non-nodal tissue (blue box) and embedded in dense ECM. (CREDIT: Nature)
This remarkable atlas's relevance is amplified by the fact that cardiovascular diseases stand as the leading cause of death worldwide. Every year, about 20,000 electronic pacemakers are implanted in the UK alone to manage these disorders. However, these devices can often be ineffective and susceptible to complications and side-effects.
A deeper understanding of the biology of the cells of the conduction system and how they differ from muscle cells will pave the way for therapies aimed at bolstering cardiac health. Additionally, it could lead to the development of targeted treatments for arrhythmias, or irregular heartbeats.
Another significant achievement of the research team was the development of the computational tool called Drug2cell. The tool predicts drug targets and possible side effects. It leverages single-cell profiles and the 19 million drug-target interactions found in the EMBL-EBI ChEMBL database.
"We often don’t fully know what impact a new treatment will have on the heart and its electrical impulses - this can mean a drug is withdrawn or fails to make it to the market. Our team developed the Drug2cell platform to improve how we evaluate new treatments and how they can affect our hearts, and potentially other tissues too. This could provide us with an invaluable tool to identify new drugs which target specific cells, as well as help to predict any potential side-effects early on in drug development," said Dr. Michela Noseda, Senior Lecturer in Cardiac Molecular Pathology at the National Heart and Lung Institute, Imperial College London, a Coordinator of the Human Cell Atlas Heart BioNetwork, and a lead author of the study.
In an unexpected turn of events, Drug2cell identified that pacemaker cells express the target of certain medications, such as GLP1 drugs, which are used for diabetes and weight loss. These drugs are known to increase the heart rate as a side-effect, the mechanism of which was previously unclear. The study suggests that the increase in heart rate might be due, in part, to these drugs' direct action on pacemaker cells, a finding also demonstrated in an experimental stem cell model of pacemaker cells.
Dr. Kazumasa Kanemaru, joint first author and Postdoctoral Fellow in the Gene Expression Genomics team at the Wellcome Sanger Institute, shed light on the importance of understanding these mechanisms. He said, “The mechanism of activating and suppressing pacemaker cell genes is not clear, especially in humans. This is important for improving cell therapy to facilitate the production of pacemaker cells or to prevent the excessive spontaneous firing of cells. By understanding these cells at an individual genetic level, we can potentially develop new ways to improve heart treatments.”
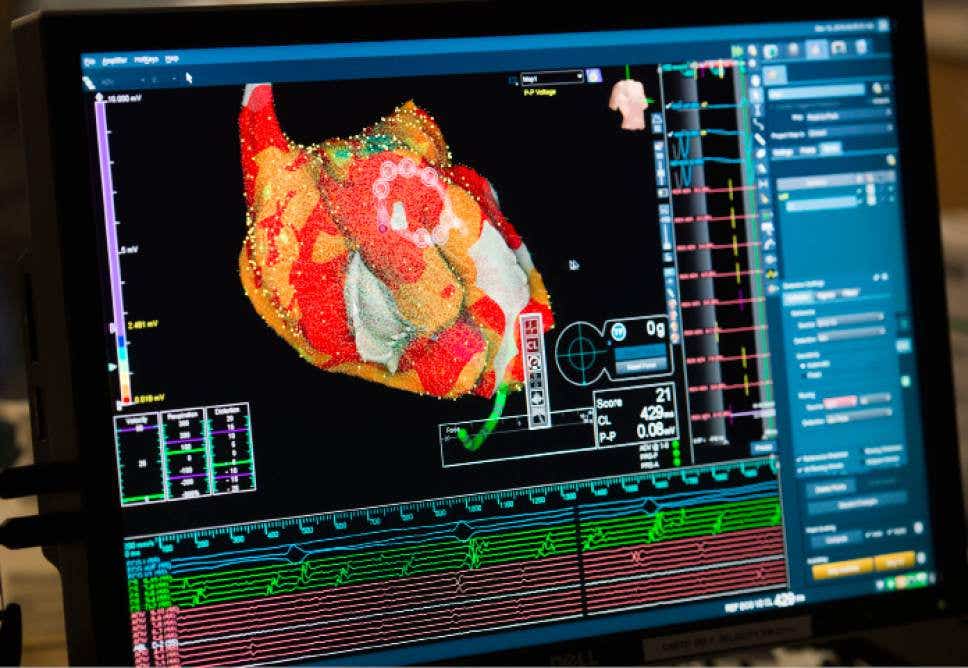
Profiling of cardiac cells. UMAP representation of from the eight regions showing the fine-grained cell state labels. The data were integrated based on their gene expression (left) or chromatin accessibility (right) with accounting for batch effects and embedded in two-dimensional UMAP space. (CREDIT: Nature)
Amid the study's key findings, two discoveries stand out: the unexpected link between conduction system cells and glial cells, and the identification of an immune structure on the heart's outer surface.
Glial cells, traditionally found in the brain and part of the nervous system, have been largely unexplored within the heart. This research suggests that glial cells are in physical contact with conduction system cells, playing an essential supporting role: they communicate with the pacemaker cells, guide nerve endings to them, and support their release of glutamate, a neurotrans
For more science and technology stories check out our New Discoveries section at The Brighter Side of News.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get the Brighter Side of News' newsletter.



