Ultrasound therapy shows promise in reversing diabetes without drugs
Researchers show ultrasound could prevent or reverse diabetes, offering a non-drug, non-invasive treatment option.
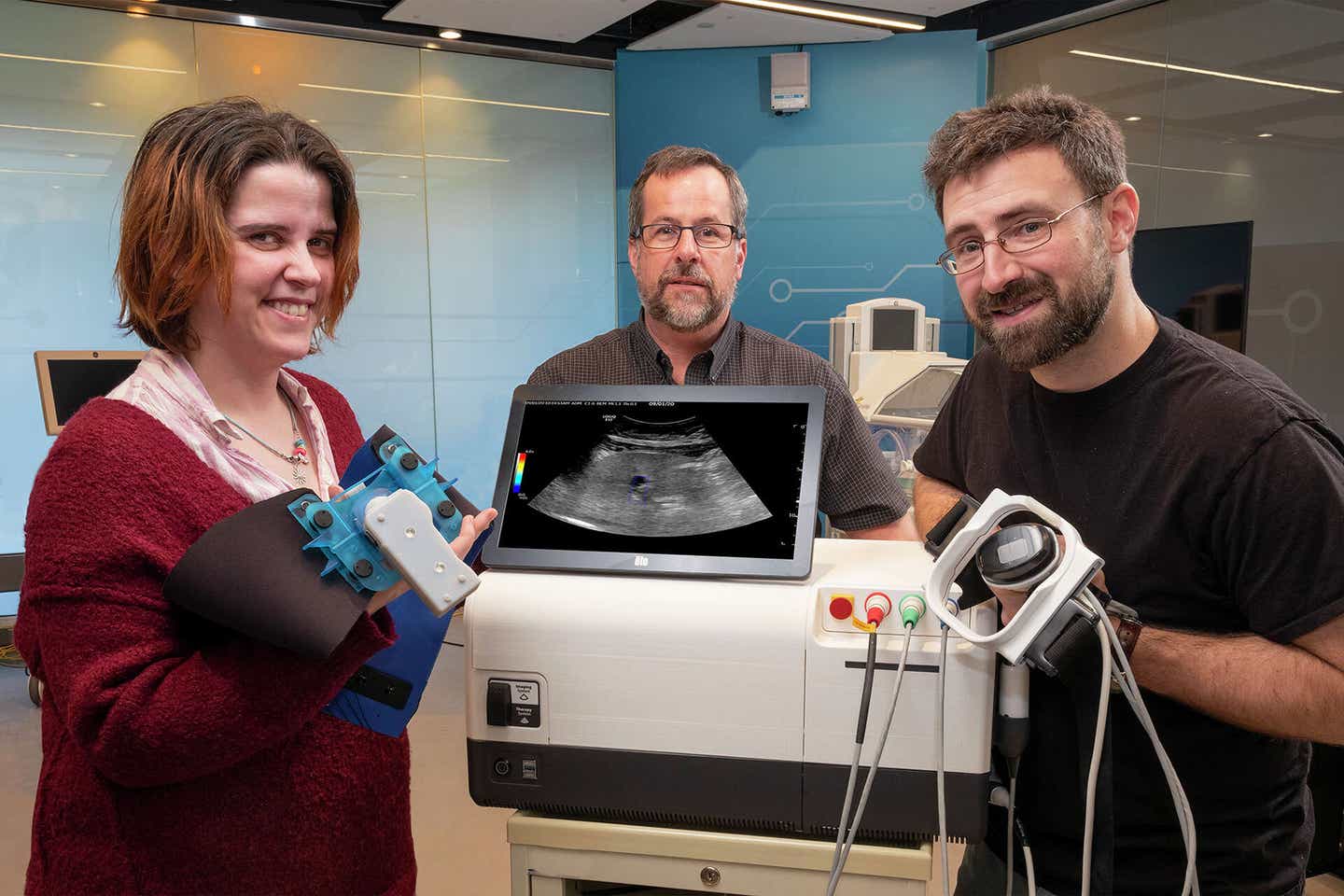
Pictured (left to right): GE Research’s Victoria Cotero, Senior Scientist in Biosciences; Jeffrey Ashe, a senior electrical engineer; and Christopher Puleo, a senior biomedical engineer, around a prototype of the Research Lab’s ultrasound modulation device at GE’s research campus in Niskayuna, NY. (CREDIT: General Electric)
The idea of treating chronic illnesses with sound waves might sound futuristic, but scientists are showing it could soon be reality. A team led by GE Research, working with partners at the Feinstein Institutes for Medical Research, UCLA, Yale, and Albany Medical College, has made headway in preventing or even reversing diabetes in animal models by using focused ultrasound.
Their findings, published in Nature Biomedical Engineering, point to a new way of controlling a disease that affects hundreds of millions worldwide.
Rethinking Diabetes Care
More than 650 million adults are obese across the globe, and obesity is one of the strongest risk factors for developing diabetes. It is often linked to inflammation, impaired nerve activity, and poor metabolic function. Today, managing diabetes relies heavily on medications, insulin injections, and careful monitoring of blood sugar levels. Despite decades of research, long-lasting therapies that stop or reverse the disease remain out of reach.
That may be changing. GE Research has spent six years developing a way to stimulate the nervous system with ultrasound instead of surgery or implanted devices. Ultrasound, already widely used for imaging, can be directed to specific parts of the body to activate nerve pathways that influence metabolism.
“We have shown that ultrasound can be used to prevent or reverse diabetes in these preclinical studies,” said Christopher Puleo, senior biomedical engineer at GE Research and co-lead of the study. “We’re now in the midst of human feasibility trials with a group of Type-2 diabetic subjects, which begins our work toward clinical translation.”
How Ultrasound Works Inside the Body
The team’s method is non-invasive. Short daily treatments—lasting only about three minutes—were shown to help stabilize blood sugar in animal studies. The ultrasound beams were directed to the liver area, a key control center for glucose and insulin regulation. In obese mice fed a high-fat, high-sugar diet, ultrasound slowed weight gain, reduced harmful fat levels in the blood, and restored balance to adipokines, hormone-like messengers that often go haywire during obesity. Inflammation in the liver also dropped, and fewer immune cells crowded the tissue.
Related Stories
- Experimental diabetes drug delivers a striking 44% reduction in body fat
- Common diabetes drug may slow aging by 18 years, study finds
Researchers believe this works by nudging nerve cells through tiny mechanical effects. “Our studies indicate that the focused ultrasound activates neurons through ion channels that are sensitive to mechanical forces,” explained Dino Di Carlo, professor of bioengineering at UCLA. While the exact mechanism is still being mapped out, the evidence shows clear benefits in glucose control and metabolic balance.
A Collaborative Effort
What makes this work stand out is the scale of collaboration. After early prototype experiments at GE showed promise, funding from DARPA’s Biological Technologies Office expanded the project to multiple labs. UCLA’s Di Carlo Lab explored how ion channels respond to sound waves.
Albany Medical College used electrodes to directly measure how nerves react. At the Feinstein Institutes, scientists confirmed results in different disease models, while Yale’s Herzog Lab applied advanced glucose clamp techniques to track blood sugar control.
“This exciting research is a major step forward to harness a novel approach of using ultrasound stimulation and bioelectronic medicine,” said Sangeeta Chavan, professor at the Feinstein Institutes. Her colleague Stavros Zanos added that the work helps “mechanistically bridge short-term and long-term physiological and metabolic effects of neuromodulation,” providing insight into how these therapies can be optimized.
Toward Human Trials
Although the results are promising, researchers are cautious. Most of the studies so far have been in animal models, and human testing has only just begun. “Even though we already have a large variety of antidiabetic medications to treat high glucose levels available to us, we are always looking for new ways to improve insulin sensitivity,” said Raimund Herzog, associate professor of endocrinology at Yale. If ultrasound proves successful in people, it could become an entirely new tool in diabetes care.
Victoria Cotero, lead author of the study from GE, highlighted that both genetic and diet-induced models of diabetes responded well to ultrasound. “The treatment was able to improve both glucose tolerance and insulin resistance,” she noted. The next challenge is fine-tuning how often treatments are needed and what types of ultrasound pulses work best. “We’re still determining the frequency of treatments that is needed to maintain the reversal of diabetes,” explained Jeffrey Ashe, senior electrical engineer on the project.
Practical Implications of the Research
The prospect of treating diabetes without daily injections or multiple medications could transform the lives of millions. Beyond diabetes, the method may also have broader applications for obesity-related conditions, including heart disease and liver problems. Damian Shin of Albany Medical College summed up the excitement: “If substantiated, our work could lead to an innovative, non-invasive way to treat Type-2 diabetes. We’re proud to have helped lay the foundation for future clinical studies.”
If confirmed in clinical trials, ultrasound neuromodulation could add a completely new option for managing diabetes, offering a treatment that doesn’t rely on drugs or needles. This non-invasive method may also help address obesity-related health problems such as liver inflammation and heart disease.
For patients, it could mean simpler, more comfortable care. For physicians, it could provide another tool to tailor treatments for individuals who don’t respond well to current medications. In the long run, this research may help reduce the global burden of diabetes and related chronic conditions.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.