Over-the-counter health supplement may hold the key to rebuilding damaged lungs
Zinc’s role in lung repair offers hope for reversing damage in idiopathic pulmonary fibrosis, a deadly lung disease.

Zinc transporter protein helps lung stem cells repair damage in IPF, opening the door to new treatments. (CREDIT: Shutterstock)
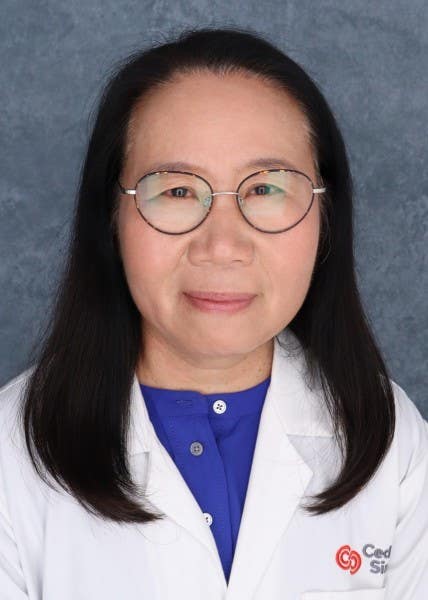
Scientists at the Women’s Guild Lung Institute at Cedars-Sinai have uncovered a surprising link between zinc and the lung’s ability to repair itself, offering hope to people living with idiopathic pulmonary fibrosis (IPF). This progressive lung disease scars lung tissue, making breathing more difficult over time. Affecting roughly 100,000 Americans, IPF is often fatal within three to five years of diagnosis, and right now there’s no cure.
In the new study, published in The Journal of Clinical Investigation, researchers found that a loss of the zinc transporter protein SLC39A8—known as ZIP8—in key lung stem cells may be driving the disease’s progression. These cells, called type 2 alveolar epithelial cells (AEC2s), help repair and regenerate lung tissue. Without ZIP8, they can’t bring zinc into the cell, and without zinc, their ability to renew and replace damaged tissue sharply declines.
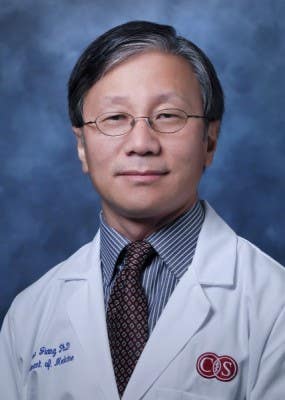
“This study has the potential to be a game changer,” said Dr. Paul Noble, chair of the Department of Medicine and co-senior author. “We identified a root cause of IPF-related lung damage and a potential therapeutic target that might restore the lungs’ ability to heal themselves.”
How the Discovery Came Together
To understand how ZIP8 loss impacts lung repair, the team worked with both human lung tissue from IPF patients and laboratory models using mice. They also grew miniature lung organoids—tiny versions of lungs created from patient tissue—to watch the regeneration process up close.
When AEC2s had ZIP8, they absorbed zinc and multiplied, forming new colonies of healthy cells. Without it, the cells stalled, struggling to rebuild damaged tissue. “The cells without ZIP8 didn’t have a way to draw zinc in, so they formed fewer colonies,” explained first author Dr. Carol Liang.
Related Stories
- Scientists discover why long COVID affects lungs differently
- Researchers develop urine test for early detection of lung cancer
In mice, deleting the ZIP8 gene from these lung stem cells not only slowed regeneration but also increased scarring. However, when researchers supplemented the mice’s diet with zinc, lung fibrosis improved.
Why Zinc Matters
The study showed zinc doesn’t act alone—it works through a chain reaction. Once inside the cell, zinc helps boost two molecules, NAD+ and Sirtuin1, both of which are linked to tissue repair and healthy aging. “Ours is the first to identify the detailed function of zinc in lung biology, specifically in IPF,” said co-senior author Dr. Dianhua Jiang.
Restoring zinc levels and activating Sirtuin1 in damaged lung tissue could, in theory, revive the lung’s self-repair system. That’s a huge leap forward compared to current treatments, which focus mostly on slowing disease progression rather than repairing damage.
The Road Ahead
While the research offers hope, more work is needed before zinc-based treatments can be offered to patients. Scientists still don’t know why ZIP8 is lost in the first place, and they need to test whether zinc supplements—possibly combined with NAD+ and Sirtuin1 activators—can safely reverse lung damage in people with IPF.
Liang says answers to these questions could help thousands: “We hope to continue our research and ultimately develop a safe and effective treatment for this disease.”
The potential of this work is especially significant given the lack of effective therapies for IPF. The discovery of the ZIP8 pathway adds to a growing understanding of how lung cells repair themselves, and it may lead to treatments that don’t just slow the disease, but actually restore lung function.

Practical Implications of the Research
If further studies confirm these findings in humans, future IPF treatments could go beyond simply managing symptoms—they could help rebuild damaged lungs. This would not only extend life expectancy but also improve day-to-day quality of life, reducing the need for lung transplants.
Such advances could also guide therapies for other lung conditions where tissue repair is impaired, potentially changing how doctors approach respiratory disease as a whole.
What are the stages of lung cancer?
According to the Cleveland Clinic, cancer is staged based on the size of the initial tumor, how far it extends into surrounding tissue, and whether it has spread to lymph nodes or other organs. Each type of cancer follows its own staging guidelines.
Lung cancer staging
Each stage of lung cancer can include several combinations of tumor size and spread. For example, a Stage III cancer may have a smaller primary tumor than a Stage II cancer, but other factors can make it more advanced. The general stages are:
- Stage 0 (in-situ): Cancer is limited to the top lining of the lung or bronchus and has not spread within or outside the lung.
- Stage I: Cancer remains confined to the lung.
- Stage II: Cancer is larger than Stage I, has spread to lymph nodes inside the lung, or there are multiple tumors in the same lobe.
- Stage III: Cancer is larger than Stage II, has spread to nearby lymph nodes or structures, or multiple tumors are present in a different lobe of the same lung.
- Stage IV: Cancer has spread to the other lung, the fluid around the lung, the fluid around the heart, or distant organs.
Limited vs. extensive stage
Although small cell lung cancer (SCLC) is now staged from I through IV, it is sometimes described as either limited or extensive stage based on whether the cancer can be treated within a single radiation field.
Limited stage SCLC is confined to one lung and may involve lymph nodes in the middle of the chest or above the collarbone on the same side. Extensive stage SCLC has spread widely within one lung or to the other lung, lymph nodes on the opposite side, or other areas of the body.
What are the symptoms of lung cancer?
Most symptoms of lung cancer are similar to those of other, less serious illnesses. Many people have no symptoms until the disease is in an advanced stage. When symptoms do occur, they may include a cough that doesn’t go away or gets worse over time. Other signs can be shortness of breath, chest pain or discomfort, and wheezing.
Some people may cough up blood or develop hoarseness. Loss of appetite, unexplained weight loss, and unexplained fatigue are also common. Additional symptoms can include shoulder pain or swelling in the face, neck, arms, or upper chest, which may be due to superior vena cava syndrome.
In certain cases, a person may have a small pupil and drooping eyelid on one side of the face, along with little or no sweating on that side—a condition known as Horner’s syndrome.
Risk factors for lung cancer
Smoking is the leading risk factor for lung cancer. Experts estimate that about 80% of lung cancer deaths are linked to smoking cigarettes, cigars, or pipes. Other risks include exposure to secondhand smoke and harmful substances such as air pollution, radon, asbestos, uranium, diesel exhaust, silica, and coal products.
Having prior radiation treatments to the chest, such as for breast cancer or lymphoma, can also increase risk. A family history of lung cancer is another contributing factor.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.