Alpha cells produce GLP-1, like Ozempic drugs, study finds
Duke researchers reveal alpha cells produce GLP-1, reshaping diabetes research and offering new paths for treatment.
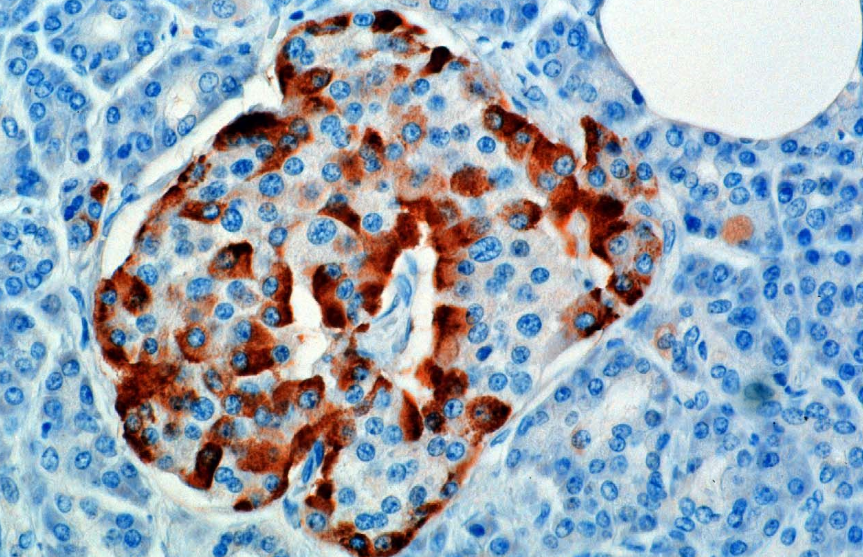
Alpha cells in the pancreas produce GLP-1, reshaping our understanding of blood sugar control and diabetes care. (CREDIT: Wikipedia / CC BY-SA 4.0)
For years, the pancreas has been being taught in biology class as an easy system: insulin lowers blood sugar, and glucagon raises it. But that's much too simple, new research says.
Scientists at Duke have discovered that pancreatic alpha cells, which were once thought to only secrete glucagon, also release another significant hormone called GLP-1. This hormone plays a critical role in insulin release and may be utilized to understand how the body handles glucose.
Beyond Glucagon
Alpha cells have long been understood to be glucagon factories, telling the liver to discharge sugar during fasting or exercise. But there had been suggestions from previous work that such cells also make GLP-1, a more widely known hormone of the gut. GLP-1 is involved in causing insulin release and is already the inspiration behind blockbuster diabetes drugs Ozempic and Mounjaro.
The fundamental question was whether alpha cells truly produce the bioactive form of GLP-1 — the form that actually binds to receptors and stimulates insulin — or if earlier findings were simply catching inactive fragments.
Measuring With Precision
To clear up the confusion, Duke University School of Medicine scientists created a new technology: a mass spectrometry test to distinguish between bioactive GLP-1 and its inactive form. That gave them, for the first time, a clear picture of what alpha cells were actually making.
Their findings were dramatic. Human pancreas tissue contained much more active GLP-1 than did mouse tissue. Even accounting for the fact that humans have more alpha cells in total number, the gap held. The results suggest that GLP-1 has a greater function in regulating human blood sugar levels than was initially believed.
Dr. Jonathan Campbell, the senior scientist, put it this way: "Alpha cells are more diverse than we believed. They can modulate their hormone secretion in the direction of beta cells to maintain blood sugar homeostasis."
When One Door Closes, Another Opens
The scientists then performed experiments on mice to determine what happens when alpha cells are forced into a shift in direction. Glucagon is typically made with the help of an enzyme called PC2, while GLP-1 is made by another enzyme, PC1. If PC2 was blocked, researchers suppressed production of glucagon — but alpha cells didn't simply shut down. Instead, they upregulated PC1 and boosted GLP-1 production.
This unexpected alteration had powerful consequences. Rather than destroying insulin secretion, it reinforced it. The animals secreted greater amounts of insulin and controlled their blood sugar better than they did originally.
Campbell explained the surprise: "We thought that deleting glucagon would destroy insulin secretion by disrupting alpha-to-beta cell interaction. Instead, it made it stronger. GLP-1 filled the gap, and as it turns out, it's a more potent insulin stimulator than glucagon."
Stress Testing the System
In a series of experiments to prove it, the researchers knocked out both enzymes in mice, halting production of glucagon and GLP-1 at the same time. The result was startling. The animals lost the ability to regulate glucose properly, and insulin release fell apart. This confirmed that at least one of the two hormones must be present for the pancreas to work.
The investigators also noted that alpha cells increased GLP-1 output under certain metabolic stresses, such as when the animals were fed high-fat diets. However, the increase was modest, indicating limitations to the body's own failsafe mechanism.
The mouse studies were only the start. With islets taken from 38 human pancreas donors and gifted to the researchers, they learned more. GLP-1 levels varied widely among individuals, but there was one clear pattern: women's islets released more GLP-1 than men's. Those higher values were linked to healthier insulin reactions.
This sexual difference may also influence the ways in which men and women respond to GLP-1-based treatments, which means that future treatments may be formulated taking these differences into account.
A New View of the Pancreas
The image is of an extremely versatile organ. Alpha cells are not dedicated to a single function. Instead, they have the ability to flip-flop between glucagon and GLP-1 synthesis, based on which enzyme they are using. In the mouse, glucagon is the preferred option, yet in humans, GLP-1 is far more important. This dual ability gives the pancreas flexibility to respond to minor variations in blood sugar.
This result suggests that the body contains an inherent backup plan," Campbell said. "GLP-1 is simply a much more powerful stimulus to beta cells than glucagon. Having the ability to switch from glucagon to GLP-1 under conditions of metabolic stress could be a critical mechanism by which the body controls blood sugar."
Practical Implications of the Research
These findings could change the way doctors treat type 2 diabetes. GLP-1-mimicking drugs already treat millions of patients with blood glucose lowering and weight reduction. Finding alpha cells make GLP-1 expands the hope to discover ways to boost this internally. These therapies could restore insulin release in patients with deteriorating beta cells.
The sex differences that scientists have observed are leading the way to more tailored medicine. If women actually do secrete more GLP-1 than men, doctors can someday use those natural variations to tailor treatments.
The study also underlines the importance of taking account of more than animal models. Mouse experiments are informative, but the much more potent action of GLP-1 in human tissue shows the worth of human information when designing therapies.
By revealing that alpha cells not only produce glucagon but also are versatile messengers, the research opens the door to new methods of optimizing blood glucose control and fighting diabetes in more targeted and more effective ways.
Research findings are available online in the journal Science Advances.
Related Stories
- Weight-loss surgery outperforms GLP-1 drugs for diabetes and obesity, study finds
- GLP-1 diabetes drugs like Ozempic found effective against migraines
- New research shows risk of muscle loss with Semaglutide use
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joseph Shavit
Writer, Editor-At-Large and Publisher
Joseph Shavit, based in Los Angeles, is a seasoned science journalist, editor and co-founder of The Brighter Side of News, where he transforms complex discoveries into clear, engaging stories for general readers. With vast experience at major media groups like Times Mirror and Tribune, he writes with both authority and curiosity. His writing focuses on space science, planetary science, quantum mechanics, geology. Known for linking breakthroughs to real-world markets, he highlights how research transitions into products and industries that shape daily life.



