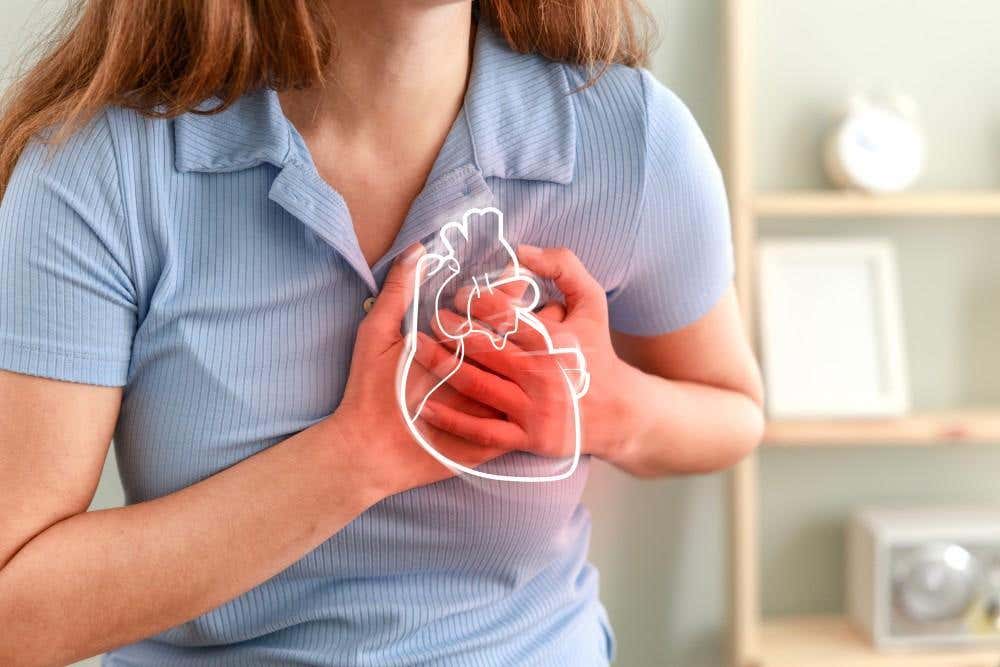
Blocking a single enzyme could help prevent heart disease and diabetes
Blocking the enzyme IDO1 helps restore cholesterol balance in immune cells, offering a new approach to fighting chronic disease.
A new study finds that blocking a key enzyme can restore cholesterol uptake in immune cells, offering a powerful tool to fight heart disease. (CREDIT: CC BY-SA 4.0)
Maintaining a healthy immune system depends on the body’s ability to control inflammation. But when this process spirals out of balance, it can damage cells and drive serious diseases like heart disease, cancer, and diabetes. At the center of this problem are immune cells called macrophages, which play key roles in regulating inflammation, cholesterol metabolism, and tissue health. When their function breaks down, the risk of chronic disease rises sharply.
The Crucial Role of Macrophages
Macrophages serve as frontline defenders, responding to pathogens, clearing debris, and coordinating the immune response. They also maintain balance in tissues by managing inflammation and metabolizing lipids. One of their most important tasks is regulating cholesterol—absorbing it, breaking it down, storing it safely, and transporting it out of the body when needed. This delicate system depends on specific transporters and enzymes that keep cholesterol from building up.
One of the key players in this process is a receptor called SR-BI, short for scavenger receptor class B type I. This protein helps macrophages both take in and release cholesterol, preventing harmful buildup inside cells. When SR-BI is disrupted, cholesterol starts to collect, transforming macrophages into foam cells—bloated, dysfunctional cells that spark chronic inflammation and trigger diseases like atherosclerosis.
How Inflammation Derails Cholesterol Metabolism
Normally, macrophages use several pathways to manage cholesterol. They absorb it from low-density lipoprotein (LDL) particles, process it inside the cell, convert it into storage form, and finally export it with the help of proteins like ABCA1 and ABCG1.
HDL particles also play a vital role in carrying cholesterol away from tissues and back to the liver. SR-BI supports both uptake and release, creating a two-way street for cholesterol control.
But during inflammation, these processes begin to fail. Stress, injury, or infection activates inflammatory molecules such as lipopolysaccharides (LPS) and cytokines like interferon-gamma (IFNγ). These compounds reduce SR-BI expression and interfere with cholesterol absorption. As macrophages struggle to function, they contribute to disease progression rather than stopping it.
Related Stories
The Role of IDO1 in Inflammatory Breakdown
A research team led by Professor Subhrangsu S. Mandal at The University of Texas at Arlington uncovered a powerful mechanism behind this dysfunction. Their studies revealed that inflammation increases levels of an enzyme called indoleamine-2,3-dioxygenase 1, or IDO1. This enzyme breaks down the amino acid tryptophan into a molecule called kynurenine. Kynurenine, in turn, disrupts cholesterol metabolism in macrophages by reducing SR-BI expression.
“We found that by blocking the enzyme IDO1, we are able to control the inflammation in immune cells called macrophages,” Mandal explained. “By better understanding IDO1 and how to block it, we have the potential to better control inflammation and restore proper cholesterol processing, stopping many of these diseases in their tracks.”
The study showed that blocking IDO1—either by knocking it down or using inhibitors—reduced the production of kynurenine and restored the ability of macrophages to absorb cholesterol. This discovery highlights IDO1 as a potential drug target for controlling diseases driven by inflammation.
Linking IDO1 to Cholesterol and Chronic Disease
Beyond LPS, stimulation with IFNγ—a common inflammatory trigger—produced the same effects. It activated IDO1, increased kynurenine levels, and disrupted cholesterol uptake. Once IDO1 was blocked, however, macrophages recovered. These findings suggest that inflammation-induced activation of IDO1 is a shared pathway in chronic diseases such as diabetes, cancer, and cardiovascular conditions.
This insight matters because many chronic illnesses share a root cause: macrophage dysfunction and lipid imbalance. In today’s world, where processed foods, stress, and sedentary habits are widespread, the body’s lipid balance often becomes disrupted. This leads to excess fat being stored in tissues and immune cells, which sparks long-term inflammation.
Foam cells, formed from macrophages overloaded with cholesterol, are hallmarks of atherosclerosis. Their presence signals a broken system that drives heart disease and other metabolic disorders. By targeting IDO1, researchers believe it may be possible to correct this imbalance and halt disease progression before it starts.
Understanding the Broader System of Lipid Balance
Cholesterol homeostasis involves a complex network of uptake, storage, and export mechanisms. After entering macrophages, cholesterol is broken down into free cholesterol by lysosomes. The enzyme ACAT1 then re-esterifies it into cholesteryl esters (CEs), which are stored until needed. When it's time to remove it, CE is hydrolyzed, and free cholesterol is sent to external carriers like ApoA1 or HDL via ABCA1 and ABCG1.
SR-BI assists in this process by selectively taking in cholesteryl esters and exporting free cholesterol. It does this without destroying the HDL particles, making it essential for reverse cholesterol transport. While SR-BI is highly active in the liver, it also plays a vital role in macrophages, helping them manage cholesterol even during periods of stress.
Previous research showed that SR-BI can be influenced by hormones like estradiol through genetic mechanisms involving histone modifiers such as MLL2. When MLL2 was blocked, SR-BI expression fell, leading to increased cholesterol levels in mice. The new research builds on this foundation, showing that inflammation also reduces SR-BI by raising IDO1 levels.
Targeting New Enzymes to Treat Disease
In addition to IDO1, the study also explored the role of nitric oxide synthase (NOS), another enzyme linked to inflammation. The researchers found that NOS made the effects of IDO1 even worse, amplifying cholesterol metabolism problems in macrophages. This discovery suggests that therapies combining NOS and IDO1 inhibition might be more effective than targeting IDO1 alone.
“These findings are important because we know too much cholesterol buildup in macrophages can lead to clogged arteries, heart disease and a host of other illnesses,” Mandal said. “Understanding how to prevent the inflammation affecting cholesterol regulation could lead to new treatments for conditions like heart disease, diabetes, cancer and others.”
The team included postdoctoral researcher Avisankar Chini, doctoral students Prarthana Guha, Ashcharya Rishi and Nagashree Bhat, master’s student Angel Covarrubias, and undergraduate researchers Valeria Martinez, Lucine Devejian and Bao Nhi Nguyen. Together, they aim to explore how IDO1 interacts with other enzymes and whether safe inhibitors can be developed into drugs.
A Path Toward Future Therapies
This line of research opens a promising path forward. Blocking IDO1 could become a new strategy to prevent diseases caused by chronic inflammation. By restoring proper cholesterol processing in macrophages, it may be possible to reduce the risk of metabolic disorders and slow disease progression before symptoms emerge.
If scientists can find safe, effective ways to reduce IDO1 activity, patients struggling with conditions like heart disease, diabetes, or even cancer could benefit from treatments that tackle the root cause rather than just the symptoms. Understanding how inflammation reshapes cholesterol regulation in immune cells could lead to more targeted, long-term solutions for managing chronic illness.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.