Breakthrough cell therapy stops cancer by stealing its nutrients
A new cancer therapy uses engineered fat cells to outcompete tumors for nutrients, starving them and slowing disease progression.
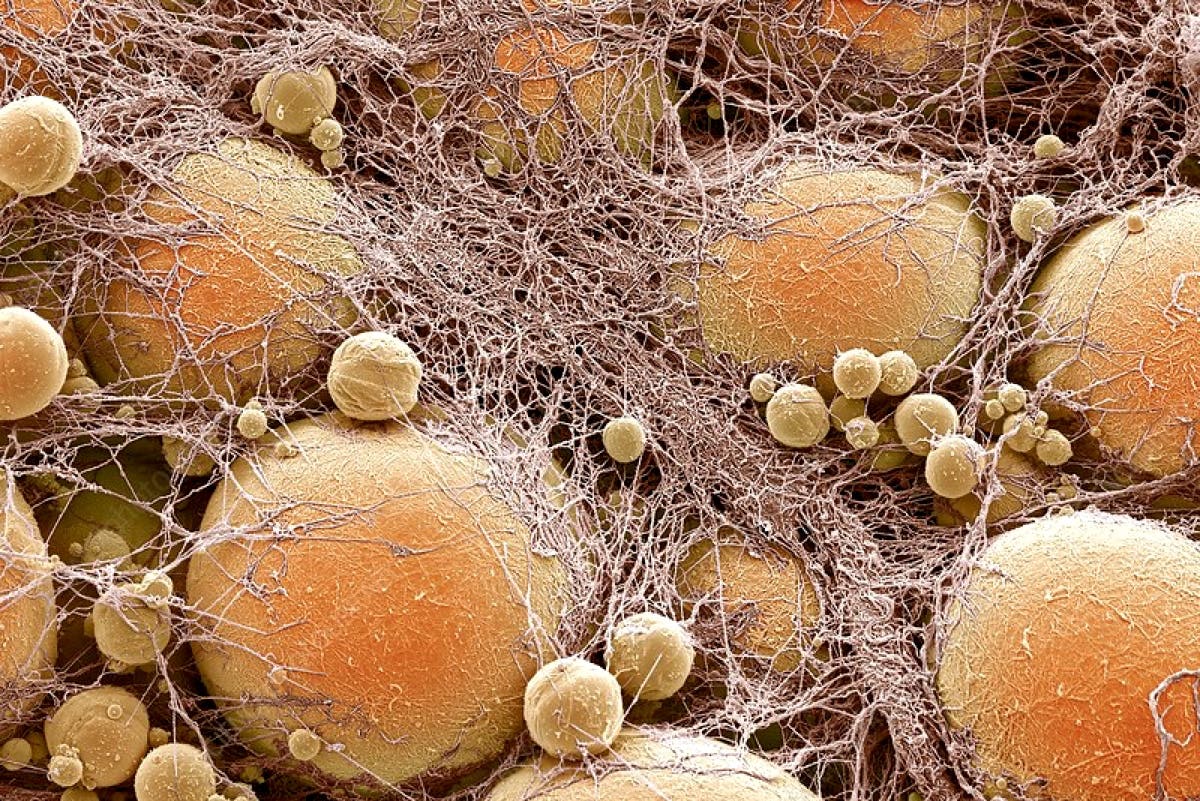
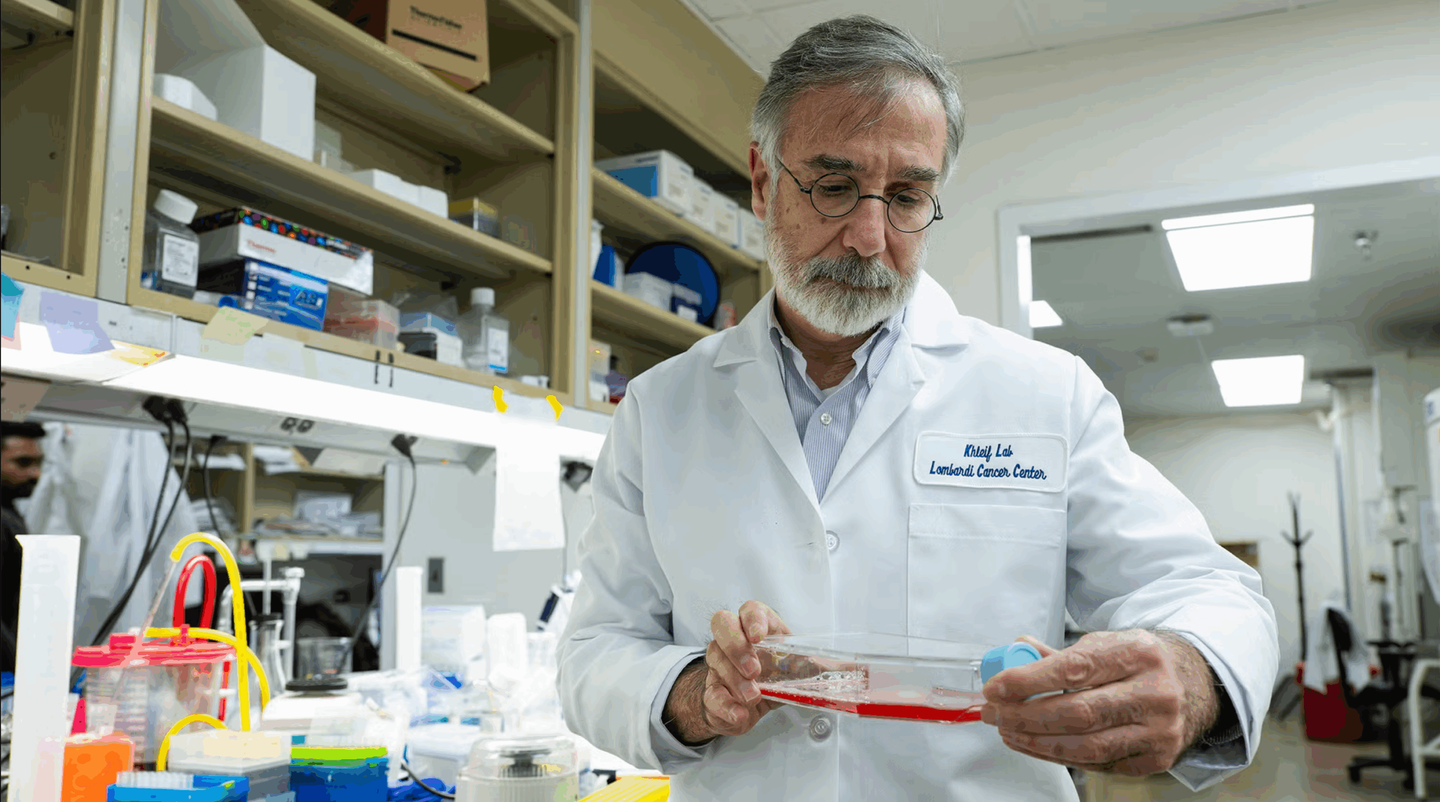
Scientists use engineered fat cells to starve tumors, halting cancer growth across multiple types in lab studies. (CREDIT: Science Photo Library)
Cancer thrives by stealing nutrients. Tumors grow fast because they hijack the body’s resources—especially glucose and fatty acids. But a new study shows there's a way to beat cancer at its own game. Scientists have discovered a treatment that uses reprogrammed fat cells to outcompete tumors for fuel. By starving tumors, these fat cells slow or even stop cancer growth.
This method, called Adipose Manipulation Transplantation (AMT), doesn’t rely on toxic drugs or radiation. Instead, it uses a clever trick—take something your body already makes and upgrade it to fight cancer from within.
Turning White Fat into Cancer Fighters
Researchers focused on white fat, which stores energy. Using gene editing, they turned it into beige fat. Beige fat doesn’t store energy—it burns it. It uses calories to make heat, just like brown fat, which becomes active in cold temperatures.
Dr. Nadav Ahituv, a geneticist from UC San Francisco, and his team used CRISPR to trigger dormant genes in white fat. These genes mimic what brown fat does when it gets cold. The key gene they found was called UCP1. When activated, it made fat cells much hungrier for nutrients—especially glucose and fatty acids.
They then tested these engineered cells, called beige fat cells, in lab dishes. The setup separated fat and cancer cells with a membrane, but they still had to share nutrients. To the researchers' surprise, most of the cancer cells died.
“In our very first trans-well experiment, very few cancer cells survived. We thought we had messed something up—we were sure it was a mistake,” said Ahituv. “So, we repeated it multiple times, and we kept seeing the same effect.” The hungry beige fat cells overpowered breast, colon, pancreatic, and prostate cancer cells. These results held up over several trials.
Real Tests in Mice Show Powerful Results
The lab results were impressive, but the team wanted to see if it worked in living creatures. So they grew clusters of engineered fat cells called organoids and implanted them next to tumors in mice.
Related Stories
Again, the results amazed them. The tumors couldn’t compete for nutrients and began to shrink. In genetically modified mice designed to develop tumors, the beige fat cells still held the upper hand. Even when implanted far from the tumor, the engineered fat cells starved the cancer cells.
This confirmed a powerful new idea: cancer could be treated by robbing it of its food supply instead of attacking it directly.
Fat That Fights with Precision
Ahituv’s team didn’t stop with general fat cells. They knew different cancers prefer different nutrients. Some need glucose. Others, like certain pancreatic cancers, rely on uridine when glucose is hard to get.
So the scientists programmed fat cells to target specific nutrients. In one experiment, they made fat cells that were hungry for uridine. Then they placed them near pancreatic cancer cells that depended on uridine for survival. The result? The cancer slowed down and stopped growing. The customized fat cells had beaten the tumor by eating its favorite food.
That’s where the therapy shows its full power: it can be tailored to the exact metabolic needs of a tumor.
Bringing the Lab to the Clinic
What makes this approach so exciting is how easy it could be to use in humans. Liposuction and fat injection are common in plastic surgery. The process to get fat from patients, engineer it in the lab, and place it back is already routine.
“We already routinely remove fat cells with liposuction and put them back via plastic surgery,” Ahituv said. “These fat cells can be easily manipulated in the lab and safely placed back into the body, making them an attractive platform for cellular therapy, including for cancer.”
And since fat is everywhere in the body, especially around the breast, the researchers tried the therapy on tissue from real breast cancer patients. They worked with Dr. Jennifer Rosenbluth, who had saved tissue samples from mastectomy surgeries.
“Because the breast has a lot of fat, we could get fat from the same patient, modify the fat, and grow it in a single trans-well experiment with that patient’s own breast cancer cells,” said Ahituv. The results matched what they’d seen before. The modified fat cells from the patient outcompeted their own cancer cells. Even more promising, when placed back in mice along with the cancer cells, the fat continued to fight.
Fat Cells Offer More Than Just Cancer Control
This therapy stands out because fat cells are easy to work with. They grow well in lab dishes. They accept gene edits without problems. And once they’re put back into the body, they don’t move around or cause immune reactions. Their behavior in the body is predictable—something doctors value.
“With fat cells, there’s less interaction with the environment, so there's very little worry of the cells leaking out into the body, where they might cause problems,” Ahituv explained. These qualities open the door for even more uses. For instance, the same type of fat cells could be designed to sense blood sugar and release insulin. This could help treat diabetes. Or they could remove extra iron in people with too much of it, a condition called hemochromatosis.
The fact that these fat cells can fight cancer even when placed far from the tumor is especially important. Some cancers, like glioblastoma in the brain, are very hard to reach with surgery or drugs. Fat cells that work from a distance might offer new hope for patients with these types of cancer.
“We think these cells could also be designed to sense glucose in the bloodstream and release insulin, for diabetes, or suck up iron in diseases where there’s excessive iron, like hemochromatosis,” Ahituv said. “The sky’s the limit for these fat cells.”
A New Direction in Cancer Treatment
This research points to a future where cancer therapy doesn't just involve killing cells. It could also involve competition—outsmarting cancer by starving it before it gets too big. Using fat cells, something the body already has in large supply, may offer a gentler and more flexible form of therapy.
The idea is simple: tumors need food. Starve them, and they shrink. By giving fat cells a makeover in the lab and returning them to the body with new hunger, researchers have found a way to weaponize one of the body’s softest tissues.
Early trials in mice and lab dishes show great promise, and since the technique uses existing medical procedures, human trials could come soon. If this method proves safe and effective in people, it could mark a major shift in how we treat cancer—by using our own cells to fight back.
Research findings are available online in the journal Nature.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.