Breakthrough drug-delivery patch promotes regeneration of heart tissue
A new timed cardiac patch delivers medicine in sequence after heart attacks, improving healing, survival, and long-term heart function.

 Edited By" Joshua Shavit
Edited By" Joshua Shavit
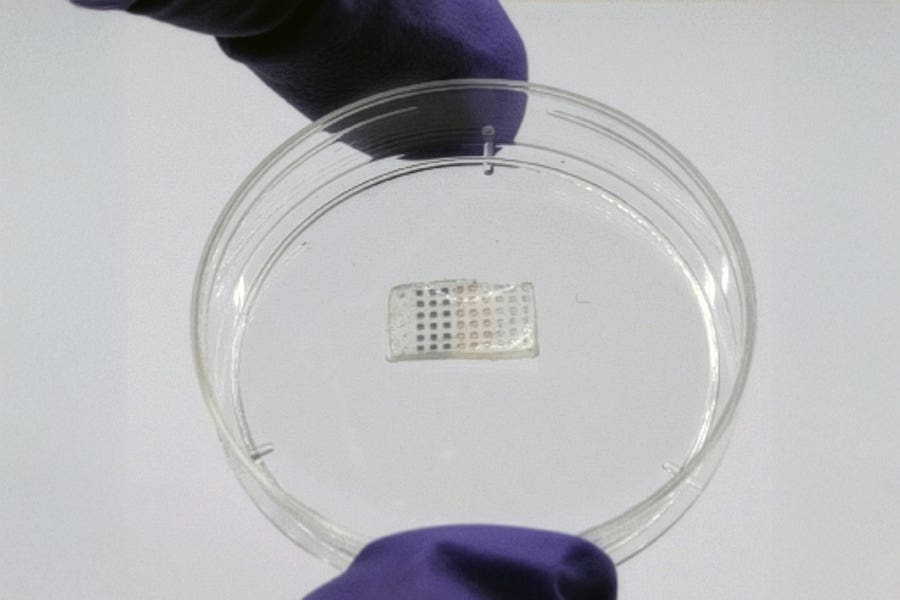
The programmable drug-delivery patch. (CREDIT: MIT)
A major heart attack can change the rest of your life. Even when doctors clear a clogged artery in time, your heart may still struggle to bounce back. Damaged muscle often turns into stiff scar tissue, and that loss of strength can slowly reshape how you move, breathe, and feel.
For years, researchers have tried to find better ways to guide the heart through its fragile stages of recovery, but most treatments arrive as one large dose that rarely fits the body’s natural schedule. Healing does not happen all at once. It follows a rhythm. New findings from MIT point to a possible solution that works with that rhythm instead of fighting it.
A Patch Designed to Work With the Heart’s Timing
A team at MIT has created a soft cardiac patch that delivers medicine in a set sequence after a heart attack. The system, known as TIMED, shortens a long scientific phrase that describes how drugs are packaged inside tiny polymer capsules and released on a planned schedule. The patch rests gently on the outer surface of the heart and acts like a guide, releasing one drug early, another a week later, and a third about two weeks after surgery.
The design is simple to picture. Each medicine sits inside a small PLGA capsule. As the capsule’s outer cap weakens, it opens at a time set by the polymer’s molecular weight. By changing those weights, researchers matched drug release to the heart’s shifting needs. Neuregulin-1 appears during days one through three, offering early support for stressed cardiac cells. Vascular endothelial growth factor follows around days seven through nine to promote new vessel growth. A TGF-β inhibitor then emerges around days twelve through fourteen to slow scar formation.
“We wanted to see if it’s possible to deliver a precisely orchestrated therapeutic intervention to help heal the heart, right at the site of damage, while the surgeon is already performing open-heart surgery,” says Ana Jaklenec of MIT’s Koch Institute for Integrative Cancer Research.
Building a Device That Moves With a Beating Organ
Anything attached to a heart must stretch, bend, and hold together under constant motion. The TIMED patch uses a tough hydrogel made from alginate and PEGDA to secure the capsules. The material stretches far beyond its original shape and stays strong enough to handle millions of beats. In lab tests, it lasted through high strain and rapid motion that went beyond what a human heart produces. Even after weeks of flexing, it held its form and kept the capsules in place. It also stored well in cold conditions for a month without major loss of strength.
That strength matters because surgeons must place the patch on soft, moving tissue during procedures like bypass surgery. The gel holds sutures, but it can also stick on its own using a hydrogel-based adhesive. Once inside the body, it slowly thins and breaks down. After a year, only a light layer remains.
“We encapsulate arrays of these particles in a hydrogel patch, and then we can surgically implant this patch into the heart. In this way, we are really programming the treatment into this material,” says lead author Erika Wang.
Early Tests Reveal Strong Signs of Healing
Before moving to animals, the team tested the device on tiny spheres of human cardiac tissue grown from stem cells. These spheres were placed under low-oxygen conditions to mimic the stress of a heart attack. When researchers added the patch, far more cells survived. Blood vessel growth improved, and collagen buildup dropped by half. Genes tied to inflammation and scarring also shifted in healthier directions.
The next step involved rats that underwent a procedure to block a major coronary artery. Four groups were compared. One group had no intervention. Another received an empty patch. A third received the same medicines by IV on days one, seven, and fourteen. The final group received the TIMED patch.
The difference stood out. Rats treated with the patch had the highest survival rate. At four weeks, survival improved by a third compared with untreated animals and by seventeen percent compared with those given the same drugs through a vein. These animals also kept more of their body weight, suggesting the local therapy reduced stress on the whole system.
Markers of heart injury like troponin I and troponin T fell by more than half after the early dose of neuregulin-1. Heart imaging showed stronger pumping action. By the end of the study, ejection fraction and fractional shortening rose more than fifteen percent above both untreated and IV-treated groups.
The tissue itself confirmed the improvement. Injured regions shrank by fifty percent. Wall thickness increased by two-thirds. The number of muscle cells in the injured area rose by more than half. Blood vessels became more organized. When fluorescent tracers were added to the patch, they stayed in the heart rather than spreading to the lungs or liver.
Toward Future Heart Treatment
Jaklenec believes the system could make a difficult recovery easier. “Our goal is to restore that function and help people regain a stronger, more resilient heart after a myocardial infarction,” she says.
Senior author Robert Langer adds, “This is an important way to combine drug delivery and biomaterials to potentially new treatments for patients.”
Neuregulin-1 and VEGF have both been tested in human trials for heart disease, which may ease the path toward a clinical study of this device. The team hopes to test the patch in larger animals. They are also exploring whether the microparticles could be placed inside stents to avoid open-chest surgery.
Practical Implications of the Research
A sequenced cardiac patch could change how you heal after a heart attack. Instead of relying on short bursts of medicine that reach the whole body, treatment could arrive right where it is needed and at the correct moment.
This device may help more patients keep their heart strength, avoid long-term scarring, and return to daily life with fewer limits. It may also open the door to other timed-release therapies for tissues that heal in stages.
The ability to match treatment to biology has the potential to reduce complications, shorten recovery, and support far better outcomes after cardiac events.
Research findings are available online in the journal Cell Biomaterials.
Related Stories
- 3D-printed heart patch made of living cells regrows damaged muscle
- New light-activated heart tissue revolutionizes heart repair
- Bee-stinger microneedle patch speeds wound healing with smart monitoring
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joseph Shavit
Writer, Editor-At-Large and Publisher
Joseph Shavit, based in Los Angeles, is a seasoned science journalist, editor and co-founder of The Brighter Side of News, where he transforms complex discoveries into clear, engaging stories for general readers. With vast experience at major media groups like Times Mirror and Tribune, he writes with both authority and curiosity. His writing focuses on space science, planetary science, quantum mechanics, geology. Known for linking breakthroughs to real-world markets, he highlights how research transitions into products and industries that shape daily life.