Eyedrop breakthrough could replace painful eye injections for retinal diseases
New eyedrop delivery system may replace invasive eye injections, offering safer, easier treatment for macular degeneration.
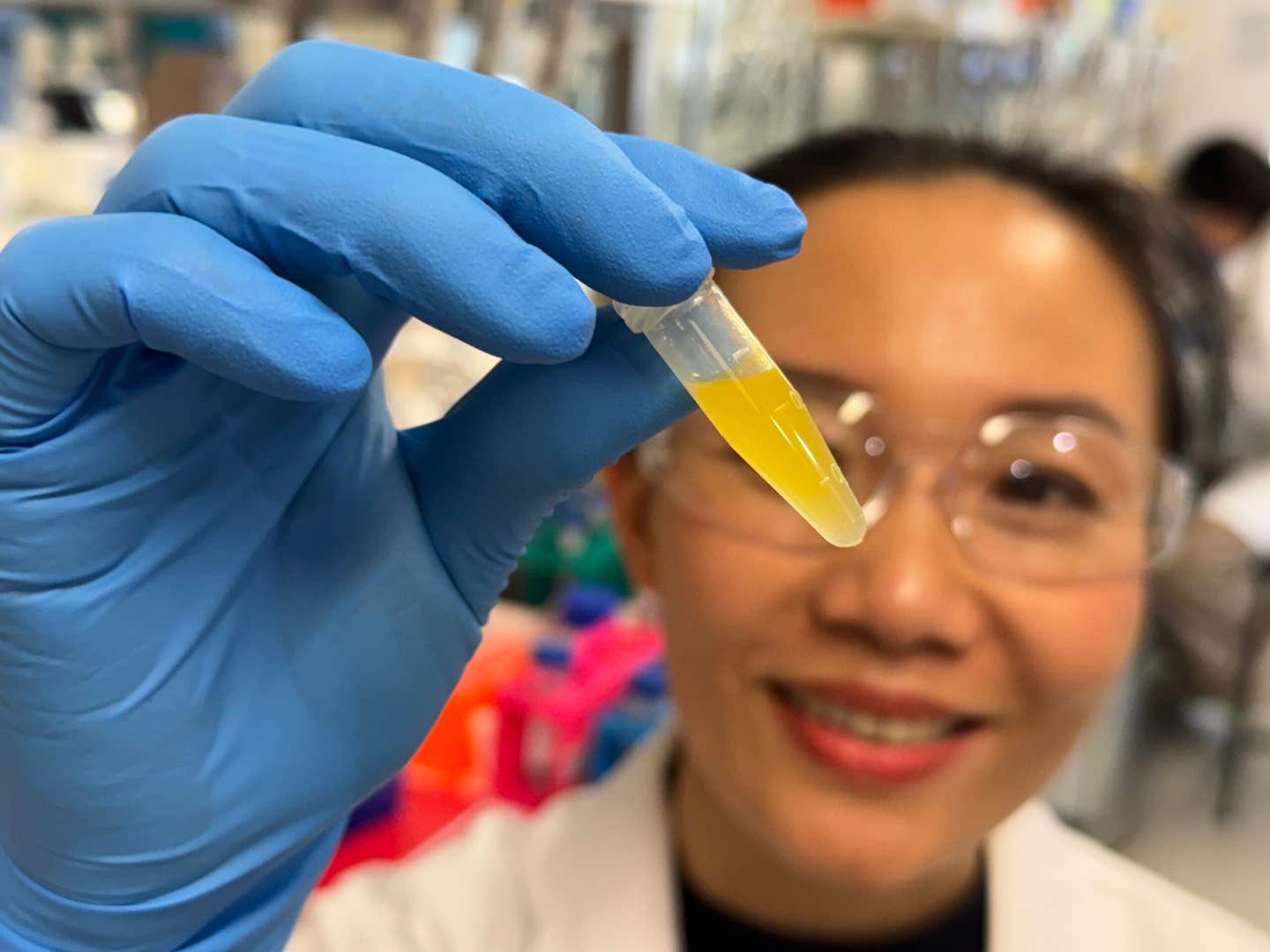
Dr Dao Nguyen examines a vial of lutein formulation developed for potential use in eyedrop treatments.
(CREDIT: Will Wright, RMIT University)
Retinal diseases such as age-related macular degeneration (AMD) and diabetic retinopathy affect millions of people globally, often leading to vision loss with minimal straightforward treatment.
Treatment options now routinely involve repeated injections directly into the eye, a painful, costly and stressful procedure for the majority of patients. However, now Australian researchers have developed an experimental eyedrop that could potentially render treatment easier, less painful and less stressful in the future.
Unleashing the Potential of Lutein
The initiative is centered on lutein, a natural anti-oxidant most commonly associated with leafy greens and brightly colored fruits. Lutein shields cells from destructive light and oxidative damage and is naturally high in concentration in the macula, which is the region of the retina used for central vision.
Although supplements in lutein are widespread, they act slowly and are of limited benefit. Patients can take 10 to 20 milligrams a day for some months before they realize any difference, and no studies have proven that oral ingestion significantly raises lutein concentration within the retina.
Getting lutein where it is needed most has been the challenge all along. The eye's natural defenses, the sclera and cornea, are formidable hurdles through which it is very hard for drug molecules in traditional eyedrops to pass through to reach the retina. The scientists wanted to overcome that obstacle by using advanced nanotechnology.
Cubosomes: Small Carriers with Great Promise
The researchers relied on cubosomes, nanoparticles with a unique internal structure that allows them to carry water-loving as well as fat-loving molecules. That structure renders them an ideal delivery system for water-insoluble lutein. By blending lutein with a cationic lipid called MO-DOTAP, the scientists developed a particle of the right size, surface charge and stickiness to remain on the eye long enough to overcome protective barriers.
They attempted two routes: intravitreal injections and naked eyedrops. Though injections contained a greater concentration in the short term, eyedrops showed steady build-up in the retina, which suggested that they can provide lutein needle-free over the long term.
To see how well the new method worked, researchers tested it on Swiss ARC mice whose retinal lutein levels were naturally low. Injections or eyedrops were given to the animals, and then their retinal tissues were analyzed. The injected eyes reached a peak within one hour but the eyedrops gradually increased lutein content within a week.
The research team also tested retinal pigment epithelial cells in vitro, which are crucial for eye health but very sensitive to oxidative damage. Stressed cells would normally have high concentrations of toxic compounds like VEGF-A and IL-6, which cause inflammation and pathological blood vessel development. When lutein cubosomes were applied, the same cells contained lower concentrations of the two compounds. The researchers credited this effect to the Nrf2/HO-1 pathway activation, a physiological antioxidant defense pathway.
A Patient-Friendly Approach
Dr. Dao Nguyen, who co-led the research at RMIT University and is currently at Deakin University, said the potential advantage is immense. "Repeated injections in the eye hurt and would be distressing to patients," Nguyen said. "If the formulation is successful, people may be able to use the eyedrop as a preventive that could possibly reduce the risk of developing late-stage diseases and the need for injections."
Associate Professor Tien Huynh, also from RMIT, noted that the platform could be used for much more than lutein. “This is a technology with broad potential. We’ve shown it can protect fragile ingredients and carry them safely to the back of the eye, which has long been a barrier for treatments,” Huynh said.
Professor Charlotte Conn and Dr. Sampa Sarkar, two of the lead researchers on the delivery mechanism, compared the cubosomes to tiny shields that guard compounds until released inside the eye. Their configuration proved not only stable at room temperature for months but also responsive to controlled release, a possibility for real-world use.
Barriers and Next Steps
The study is still in its early stages. Experiments were conducted on cell culture and healthy mice, not AMD-stricken animals or other retinal illness. Results may not be transferable to humans because of the thinner outer layer of the eye of a mouse than of humans. Some of the eyedrops in the trials failed to stay on the eye of the animal or were rubbed off, reducing their effectiveness.
Associate Professor Chi Luu, a clinician-scientist at the Centre for Eye Research Australia, said the findings were promising but cautioned that human trials were required. "This kind of approach has the potential to revolutionise the management of age-related macular degeneration. If follow-on trials confirm the safety and effectiveness of the delivery vehicle, eyedrops could eventually be applied for the treatment of early AMD and other advanced retinal diseases," Luu said.
The next step for the research team is to test the eyedrops in larger animal models before working with industry and clinical partners to develop human trials.
Practical Relevance of the Study
With success in humans, the eyedrops can potentially revolutionize the treatment of retinal disease. Instead of relying on repeated, invasive injections, patients could simply drop a treatment at home, increasing comfort and compliance.
The strategy may not only slow the progression of age-related macular degeneration but also cure other conditions such as diabetic retinopathy.
Beyond lutein, the cubosome technology may be employed as a generic delivery system for sensitive medications, and this may give rise to new eye and other disease therapies.
Research findings are available online in the journal ACS Applied Materials & Interfaces.
Related Stories
- New eye drops could replace reading glasses for millions
- Breakthrough eye drops reverse vision loss from age-related macular degeneration
- New AI tool can predict the risk of severe vision loss
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joshua Shavit
Writer and Editor
Joshua Shavit is a NorCal-based science and technology writer with a passion for exploring the breakthroughs shaping the future. As a co-founder of The Brighter Side of News, he focuses on positive and transformative advancements in technology, physics, engineering, robotics, and astronomy. Joshua's work highlights the innovators behind the ideas, bringing readers closer to the people driving progress.