First-of-its-kind drug promotes organ and heart tissue regeneration
UCLA scientist Arjun Deb develops AD-NP1, a groundbreaking antibody that helps damaged hearts and organs repair themselves.
AD-NP1, a lab-made antibody that restores the body’s natural healing power, helping the heart and other organs recover after injury. (CREDIT: Shutterstock)
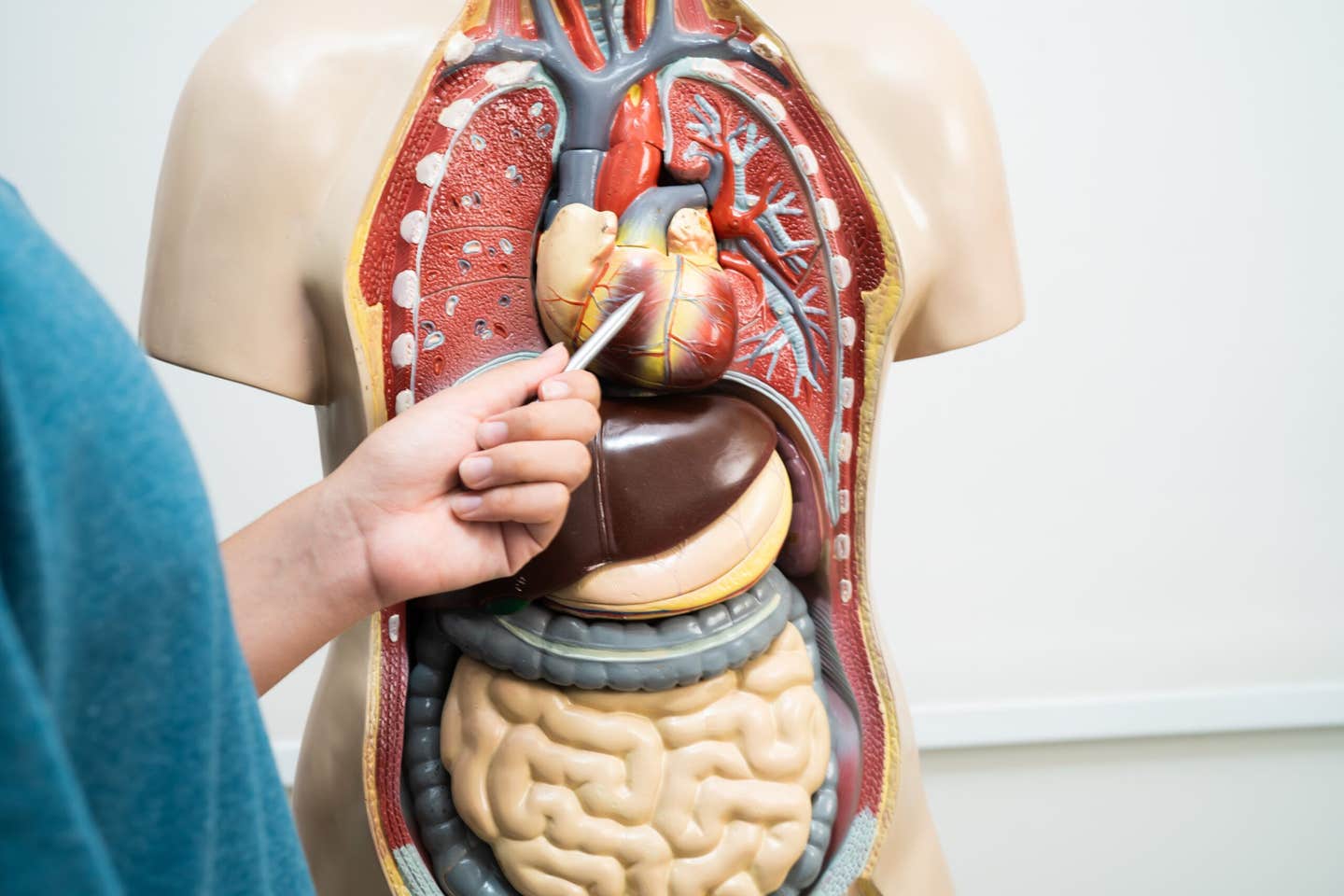
When the human body gets hurt, most tissues heal—skin closes over a wound, bone heals itself. But not all organs heal that easily. The kidneys and the heart, for example, are not as willing to heal quickly. A heart attack, for example, can lead to permanent scarring that weakens the muscle and slows its pumping action.
Researchers have been searching for years a way of making such organs repair themselves better. Now, one group at UCLA believes they've found a hopeful solution.
A Deeper Look at ENPP1 and the Heart's Energy Crisis
UCLA cardiovascular scientist Arjun Deb and his group identified a key participant in why some tissue doesn't heal: a protein called ENPP1. When Deb examined heart tissue in mice and humans after a heart attack, he observed that levels of ENPP1 spiked in the damaged tissue. That burst initiated a cascade, disrupting how cells produced energy and debilitating their function to repair tissue.
"Similar to how humans eat to get energy, cells require energy to grow and multiply and work, and it is even more critical when the tissue is injured," Deb said.
When they blocked ENPP1, the heart cells could restore their energy output, regenerate tissue, and restrict scarring. The force of the contracting heart muscle improved more effectively, preventing the heart from advancing to failure.
A New Antibody Engineered to Heal from Within
In her efforts to specifically target ENPP1, Deb's laboratory engineered a monoclonal antibody known as AD-NP1 that incapacitates the protein and increases tissue repair. Monoclonal antibodies are synthetic molecules engineered in a laboratory to mimic the body's original immune protection. In this case, AD-NP1 was engineered to target specifically only ENPP1 but not other proteins.
After having passed successful tests in mice and monkeys, the antibody was found to be both safe and effective. Now the U.S. Food and Drug Administration has paved the way for AD-NP1 to move to human clinical trials.
That milestone puts the drug that much closer to becoming a new kind of treatment—one that could help the body's own repair processes do what they are supposed to do.
Conceived Entirely Within the Public Research System
What is rare about this achievement is the way in which it was accomplished. Unlike conventional drug discoveries that rely on biotech companies or freelance investors, AD-NP1 was developed entirely within the UCLA laboratory, with no outside funding.
This work has been completely financed by tax dollars, and conducted completely within the research universe of the University of California," said Deb, who is also a professor of medicine and molecular, cell and developmental biology. "I have not accepted a penny from any private donor or firm to create this drug. I hope that this will be a model for future drug development at UCLA.
Deb's group funded themselves through the National Institutes of Health, the Department of Defense, and the California Institute for Regenerative Medicine. They personally worked through each research step over seven years, from early protein tests to FDA approval for human trials. As Deb puts it, keeping the process in a public university ensures lower prices, tighter timelines, and scientific freedom—essential advantages for innovation that ends up with the public.
Beyond the Heart: A Universal Repair Mechanism
AD-NP1's therapeutic potential goes beyond the heart. Because ENPP1 disrupts the same cellular energy pathways in many types of tissues, the drug also heals the kidneys, liver, and other organs following injury.
"When biochemical pathways to make energy in a cell are disrupted in a negative way, cellular function declines," said Deb. "That is what we saw: increased expression of ENPP1 interrupted vital pathways required for a cell to acquire energy."
By restoring those channels, AD-NP1 releases the body's own healing potential—without stem cells or man-made implants. "Rather than, you tap into the body's own healing system and hone it so as to make it so much better," explained Deb.
If human studies confirm what animal research has shown, the antibody could pave the way for a new class of drugs that enhance the repair of tissues and avoid organ failure after disease or injury.
From Bench to Bedside
AD-NP1's success is an unprecedented example of therapy development from bench to clinical trials in a single academic institution. Deb's team was able to do something that generally requires large pharmaceutical companies' resources, but all within the context of a public university.
"Cardiovascular disease still is the leading cause of death in the United States and worldwide," Deb said. "All Americans care about living healthier, longer lives free of disease. It's testament to the manner in which we finance medicine in this country that in seven or eight years in an academic laboratory in a university setting we have created a new medicine that would possibly be helpful to many with heart disease or some other form of organ damage."
Although human trials have only now started, the hope is that AD-NP1 will confirm what has been observed in animal trials: that controlling one protein could be the answer to releasing the body's potential for self-healing more powerfully.
Practical Implications of the Research
If successful in humans, AD-NP1 could launch a new generation of regenerative medicine—therapies that stimulate the body's own cells to repair organs damaged by injury, heart attack, or disease. The strength of the antibody to enhance cellular energy production should enable more rapid and complete recovery and reduce long-term disability and organ failure.
Because the drug was developed entirely within a public research infrastructure, it also demonstrates how publicly funded science can provide life-saving drugs to clinical practice without the prohibitive cost that may be fueled by private funding.
That approach could be an inspiration to universities across the nation to pursue their own stand-alone drug development with a focus on affordability and access.
Related Stories
- New light-activated heart tissue revolutionizes heart repair
- 3D-printed heart patch made of living cells regrows damaged muscle
- Internal fat may be the leading cause of heart failure, study finds
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Joseph Shavit
Science News Writer, Editor-At-Large and Publisher
Joseph Shavit, based in Los Angeles, is a seasoned science journalist, editor and co-founder of The Brighter Side of News, where he transforms complex discoveries into clear, engaging stories for general readers. With experience at major media groups like Times Mirror and Tribune, he writes with both authority and curiosity. His work spans astronomy, physics, quantum mechanics, climate change, artificial intelligence, health, and medicine. Known for linking breakthroughs to real-world markets, he highlights how research transitions into products and industries that shape daily life.