From nerves to bones: How diabetes changes the human skeleton
Diabetic nerve damage may silently weaken bones. New research reveals lost nerve signals disrupt bone growth and repair.
New study reveals how diabetes-related nerve damage weakens bones and may raise fracture risk. (CREDIT: Science Photo Library)
In diabetes, much attention goes to sugar control, insulin levels, and the threat of nerve damage. But a new study reveals something often overlooked—how the breakdown of nerve function in diabetes also harms your bones. This quiet connection, hidden deep in the body's structure, may explain why people with diabetes are more likely to suffer fractures, even without major trauma.
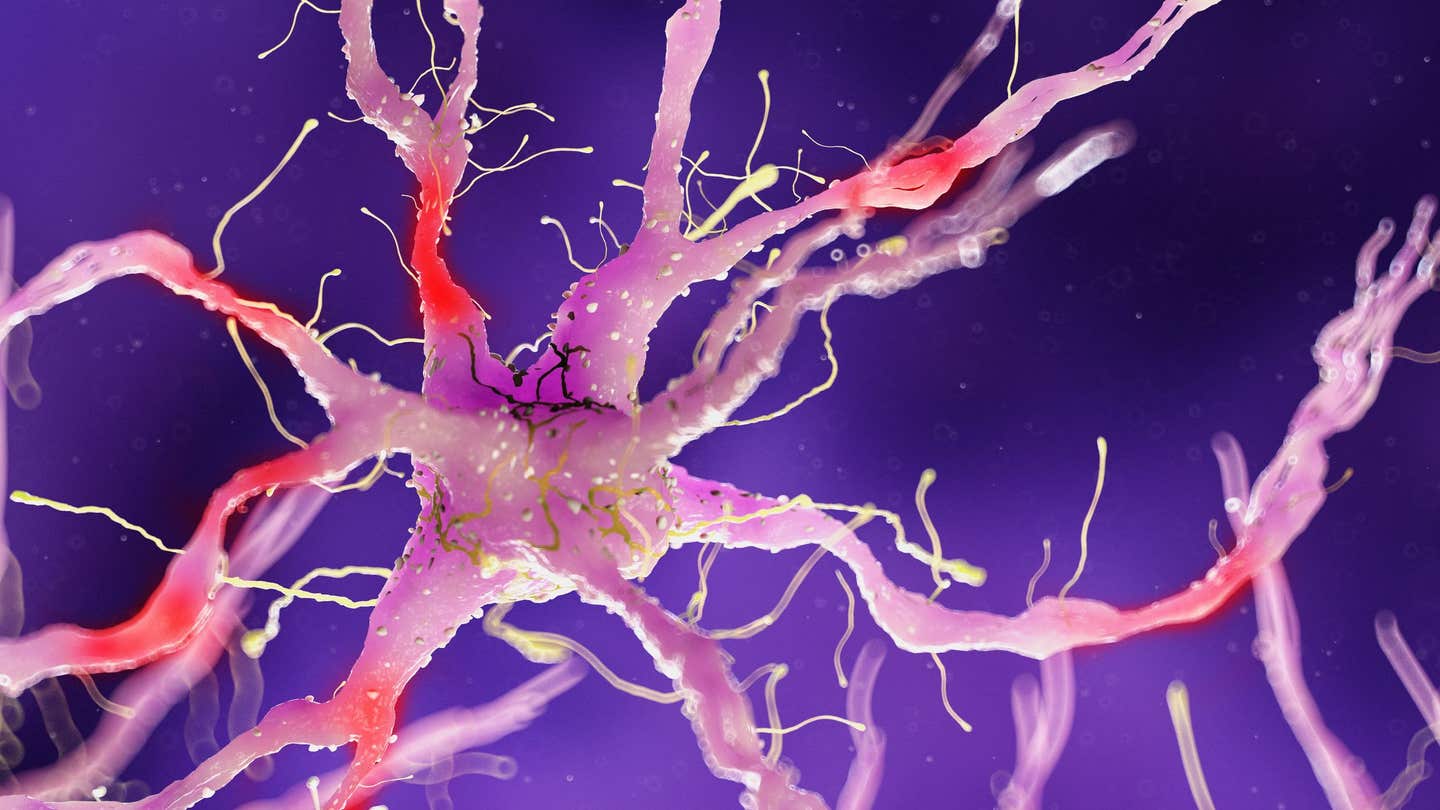
At the center of this discovery is diabetic peripheral neuropathy (DPN), a complication affecting about half of all people with diabetes. It causes nerve fibers to break down, reducing sensation and causing pain, especially in the feet and legs. But scientists are now learning that DPN may do more than harm nerves—it may disrupt the signals that help bones grow and stay strong.
A team of researchers led by Dr. Aaron James at Johns Hopkins University set out to test this idea. Their findings, published in Bone Research, uncover how nerve damage in diabetes reduces bone density and increases fracture risk—by cutting off key signals between nerve and bone cells.
Linking Nerves and Bones Through Diet
To explore this nerve-bone connection, the scientists used young male mice and fed them a high-fat diet to model type 2 diabetes. These mice developed typical signs of the disease, including weight gain, high blood sugar, and insulin resistance. But they also showed clear signs of peripheral neuropathy, such as fewer nerve endings in the skin and a weaker response to pain. What surprised researchers most was what happened inside the bones.
In the long bones of diabetic mice, nerve fiber density dropped dramatically—by as much as 76%. Two types of nerve fibers, marked by Beta-III-Tubulin and CGRP, showed reductions of 69% and 38% respectively in the periosteum, the thin membrane that covers the bone surface. This loss of nerve supply directly lined up with weaker bones. Bone volume dropped. The outer layer, or cortical bone, became thinner. The spongy inner bone, called trabecular bone, also lost mass.
“We’ve known that patients with diabetes have a higher risk of fractures, but our study shows that part of this risk may come directly from disrupted nerve-bone communication,” said Dr. James.
Related Stories
- Pistachio snacks may boost gut health for diabetes prevention, study finds
- New drug combination protects women from breast cancer and diabetes without side effects
- GLP-1 diabetes drugs like Ozempic found effective against migraines
Messages Lost in Translation
To find out how damaged nerves affect bones, the team studied the signals these nerves send. Using single-cell RNA sequencing (scRNA-Seq), they examined gene activity in both the nerve cells and bone-surrounding periosteal cells.
In healthy conditions, sensory neurons release signaling proteins like VEGFA (Vascular Endothelial Growth Factor A), BDNF (Brain-Derived Neurotrophic Factor), and CGRP (Calcitonin Gene-Related Peptide). These molecules act like messengers, telling bone cells to grow and repair. But under diabetic conditions, these messages seemed to fade.
Instead of growing into bone-forming cells (osteoblasts), periosteal cells in diabetic mice shifted toward becoming fat cells. This change in direction—known as adipogenesis—was a key sign that the bone's natural repair system was off-track.
The RNA sequencing also revealed that major cell pathways vital for bone health were suppressed in diabetes. These included WNT, TGFβ, MAPK, and mTOR signaling—pathways that control cell growth, bone repair, and balance between forming and breaking down bone. Without these signals, the bone-building process simply stalled.
A Surprising Turnaround
But then came an unexpected finding. When periosteal cells taken from diabetic mice were treated with conditioned media—fluid collected from healthy nerve cells—they bounced back. The cells began to divide and form bone tissue again. Even the MAPK pathway, once suppressed, became active once more.
“This restoration of lost communication between nerve and bone cells could be a game changer,” said Dr. James. “By targeting these neural pathways, someday we may also be able to prevent or even reverse bone deterioration in people with diabetes.”
The conditioned media worked like a lifeline. It reintroduced the signals that were missing due to nerve damage. It didn’t just stop the negative changes—it reversed them.
A Wider Horizon in Bone Research
This study opens new questions that go beyond diabetes. If nerves play such a powerful role in maintaining bone, what does this mean for other bone diseases like osteoporosis or non-healing fractures? Could nerve-targeted therapies improve recovery after injury or surgery?
The research also raises questions about how age, sex, and disease severity affect nerve-bone communication. Future studies will look at these factors and identify exactly which molecules in the nerve-derived fluid are responsible for restoring bone growth. This could lead to targeted therapies that repair bone by mimicking healthy nerve signals.
The implications could be life-changing. As populations age and diabetes rates continue to rise, bone fractures linked to poor bone health are becoming more common—and costly. Identifying the missing link between nerves and bones could offer new tools to stop fractures before they start.
Instead of focusing only on calcium, vitamin D, or hormones, future treatments may include ways to restore or replace lost nerve signals. For patients living with diabetes, this offers a glimmer of hope. The nerve pain they endure might be the first clue to deeper problems—but also a doorway to new solutions.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.