GLP-1 weight-loss drugs could help protect eyes from diabetic retinopathy
Lab study finds semaglutide boosts retinal cell survival and cuts oxidative stress markers tied to diabetic retinopathy.

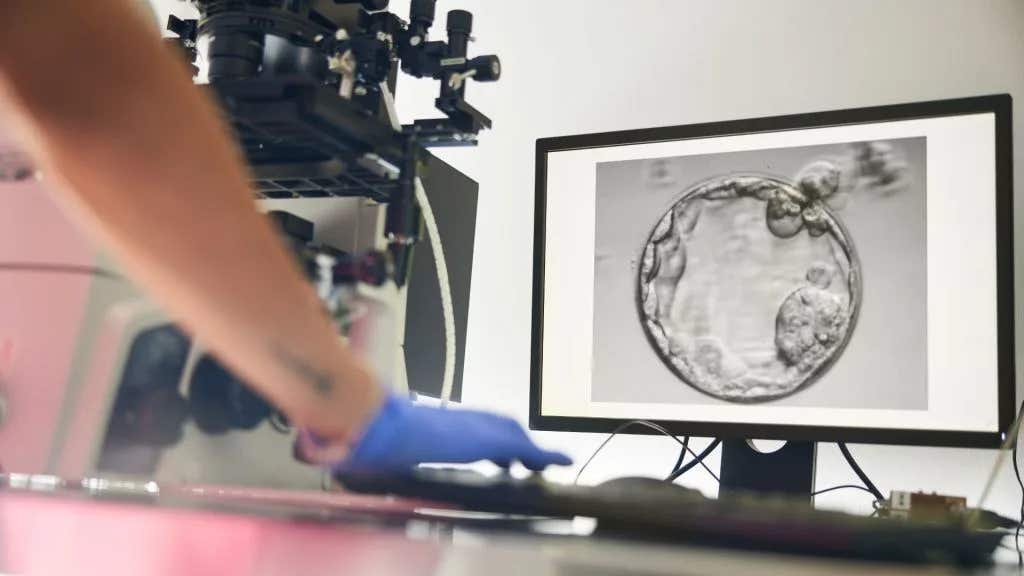
A new lab study suggests GLP-1 drugs like semaglutide may protect retinal cells from diabetes-like damage, supporting trials in patients. (CREDIT: Pharmaceutics)
Sight can slip quietly in diabetes, often before you feel anything is wrong. The damage can start in the tiny blood vessels of the retina, the light-sensing tissue at the back of the eye. Over time, high blood sugar can weaken those vessels and harm the cells around them. That process can lead to diabetic retinopathy, a common complication that can steal vision.
New research suggests a widely used class of diabetes and weight-loss drugs may help protect retinal cells from that damage, at least in early stages. The work will be presented at the annual meeting of the European Association for the Study of Diabetes in Vienna, Austria. The study focuses on GLP-1 receptor agonists, including semaglutide.
These drugs mimic the action of GLP-1, a hormone that helps the body make more insulin when needed. They also slow digestion, curb appetite, and increase feelings of fullness. Scientists have also noted that many tissues have GLP-1 receptors, and recent research suggests the drugs may have anti-inflammatory and antioxidant effects.
That extra biology matters for your eyes. Diabetic retinopathy remains a leading cause of blindness among working-age adults. The condition develops when high blood sugar damages retinal blood vessels. More than 90% of people with type 1 diabetes, and about 50% to 60% of those with type 2 diabetes, develop diabetic retinopathy.
“Diabetic retinopathy represents a major public health challenge,” said Ioanna Anastasiou of the National and Kapodistrian University of Athens in Greece, who led the research. “Globally, it is projected that over 191 million people will be affected by it by 2030, with around 56 million experiencing vision-threatening stages of the disease.
“These statistics underscore the critical need for effective screening, early detection, and, crucially, more effective treatments.”
Why the Retina Takes a Hit in Diabetes
To understand why the researchers focused on antioxidants, it helps to look at what high blood sugar does inside cells. When glucose stays high, cells can produce more free radicals. These are molecules that can damage cells. The body uses antioxidants to neutralize them, but diabetes can tip the balance toward harm.
Much of the injury in diabetic retinopathy is thought to involve this oxidative stress. Retinal endothelial cells, which line the blood vessels in the retina, can suffer under that pressure. When those cells break down, the retinal environment becomes more fragile and more likely to fail.
Researchers have debated how GLP-1 drugs fit into this story. Some studies have suggested these drugs reduce the risk of diabetic retinopathy. Other studies have suggested the drugs may increase the risk, or worsen the condition in people who already have it. That uncertainty has left clinicians and patients with mixed signals.
Anastasiou and colleagues set out to add clarity with a detailed lab study. Their goal was to see what GLP-1 receptor agonists do to retinal cells under diabetes-like conditions, and to measure the damage in concrete ways.
The Lab Setup and What Scientists Tested
The study used human retinal endothelial cells. "Our team exposed those cells to conditions meant to resemble the diabetic environment. The cells sat in media with high glucose levels and oxidative stress for 24 hours. That setup created a situation where free radicals outnumber antioxidants, which mirrors a key feature of diabetic tissue damage," Anastasiou told The Brighter Side of News.
"We then treated the cells with a range of semaglutide concentrations. After that, we ran a series of tests to evaluate cell survival and cell stress," she continued.
The results pointed in one direction. Cells treated with semaglutide were up to twice as likely to remain alive as untreated cells. The treated cells also had larger energy stores, suggesting they held onto more cellular fuel during stress.
The team also tracked several markers tied to oxidative stress and retinal damage in diabetic retinopathy. Those measures dropped sharply in semaglutide-treated cells.
Apoptosis, a form of cell death, fell from about 50% in untreated cells to about 10% in semaglutide-treated cells. The production of mitochondrial superoxide, a free radical, dropped from about 90% to about 10%. The accumulation of advanced glycation end-products, harmful compounds linked to high blood sugar, also fell substantially.
Together, those shifts suggest the treated cells handled stress better. They also suggest the drug supported cell survival during a damaging, diabetes-like challenge.
A Closer Look at The Antioxidant Signal
The researchers did not stop with survival counts. They also looked at gene activity inside the cells. Their analysis showed that genes involved in antioxidant production became more active in the treated cells compared with untreated cells.
That result supports a theory about how GLP-1 receptor agonists may protect the retina. If the drug helps boost antioxidants, the cells may neutralize free radicals more effectively. That could reduce the chain reaction of injury that leads to retinal vessel damage.
Anastasiou described the findings in simple terms. “In experiments in the lab, GLP-1-receptor agonists exerted powerful antioxidant effects which protected retinal cells against the type of damage that can occur in diabetes.
“Our study did not find that these drugs harmed the retinal cells in any way; instead, it suggests that GLP1-receptor agonists protect against diabetic retinopathy, particularly in the early stages.
“Excitingly, these drugs may be able to repair damage that has already been done and so improve sight.
“Clinical trials are now needed to confirm these protective effects in patients and explore whether GLP-1 receptor agonists can slow, or even halt, the progression of this vision-robbing condition.”
The study’s message stays focused on the lab bench. It shows what happens in a controlled cellular setting. It does not yet prove what happens in patients. Still, it offers a strong clue about a potential protective pathway.
Practical Implications of the Research
If future clinical trials confirm these effects in people, the impact could be meaningful for both patients and health systems. Diabetic retinopathy affects large numbers of people, and vision loss can reshape daily life. Protecting retinal cells early could help preserve sight for longer, especially if clinicians can identify patients at risk before symptoms appear.
The study also helps researchers address a real disagreement in the field. Some prior work raised concerns about retinopathy risk with GLP-1 drugs, while other work suggested benefits. By showing direct protective effects in retinal endothelial cells under diabetes-like stress, this research gives scientists a clearer starting point to ask why different studies have produced different signals.
For research, these findings point to a practical next step: trials that track retinal outcomes in patients using GLP-1 receptor agonists, with careful attention to stage of disease and timing. For people living with diabetes, the long-term hope is a treatment that does more than manage blood sugar. It could also help defend the tissues that diabetes quietly wears down.
Research findings are available online in the journal Pharmaceutics.
Related Stories
- Your eyes and emotions help shape your sense of temperature, study finds
- GLP-1 drugs like Ozempic and Wegovy are changing the foods Americans buy
- Alpha cells produce GLP-1, like Ozempic drugs, study finds
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Hannah Shavit-Weiner
Medical & Health Writer
Hannah Shavit-Weiner is a Los Angeles–based medical and health journalist for The Brighter Side of News, an online publication focused on uplifting, transformative stories from around the globe. Passionate about spotlighting groundbreaking discoveries and innovations, Hannah covers a broad spectrum of topics—from medical breakthroughs and health information to animal science. With a talent for making complex science clear and compelling, she connects readers to the advancements shaping a brighter, more hopeful future.