Harvard gene editing treatment corrects brain mutations and improves survival
In a major breakthrough, scientists used gene editing to correct brain mutations in mice with AHC, easing symptoms and extending life.
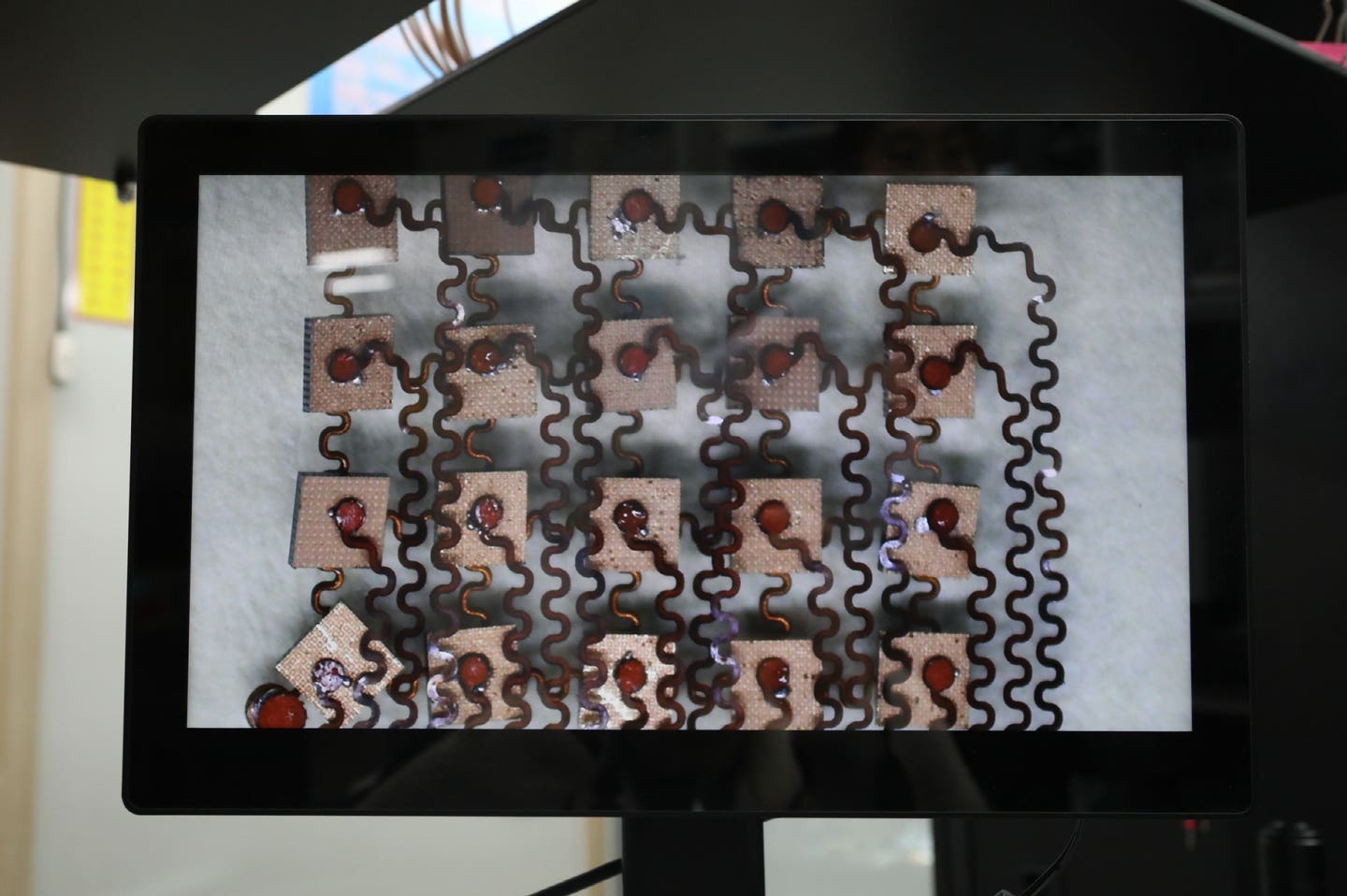
Gene editing fixed brain mutations in mice with AHC, offering hope for treating rare neurological diseases at the DNA level. (CREDIT: Cathleen Lutz, et al.)
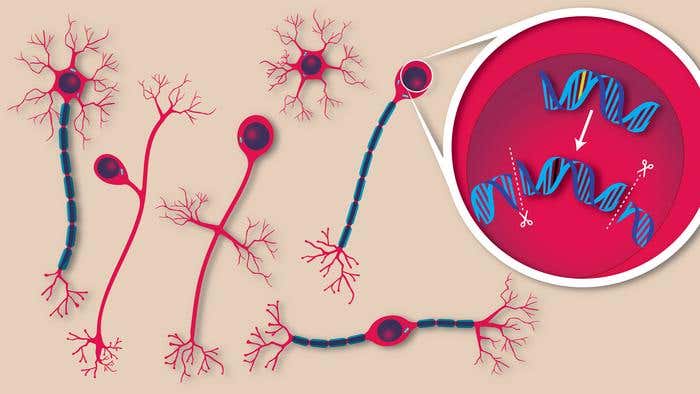
In a major step toward treating rare neurological diseases, scientists have used gene editing to correct mutations inside the brain of living mice with a single injection. This new approach, described in the journal Cell, could reshape the future for people with devastating conditions once thought untreatable.
The disorder targeted in the study is called alternating hemiplegia of childhood (AHC), a disease that strikes in infancy and causes sudden paralysis, muscle rigidity, seizures, and developmental delays. It has no cure and limited treatment options. Until now, even testing potential therapies has been a challenge, due to the complex nature of the disease and the difficulty of reaching brain cells safely and effectively.
But in this new research from Harvard University, scientists were able to not only correct the disease-causing mutation in mice but also improve symptoms and extend survival. The team used a precision gene editing method called prime editing, which alters DNA by rewriting the genetic “letters” that carry instructions inside our cells.
Targeting the Root of Neurological Disease
The scientists focused on the gene ATP1A3, which is responsible for most cases of AHC. Two mutations in this gene—D801N and E815K—have been known to cause the disorder. Using genetically modified mice that carried these mutations, researchers observed disease signs similar to those in human patients. These mice had spontaneous seizures and often died young.
To repair the mutations, scientists injected a harmless virus—called AAV9—that carried gene editing tools into the brain shortly after the mice were born. This method helped the editing tools reach a large number of neurons before damage from the disease could build up.
The result was remarkable: the faulty gene was corrected in up to 85% of brain cells. That level of correction restored protein function, reduced seizure-like behavior, and improved the mice’s movement. Most importantly, many lived longer than untreated mice. “This is a pretty big deal,” said Markus Terrey, a neuroscientist at The Jackson Laboratory (JAX), who co-led the study. “Five years ago, people thought fixing DNA inside the brain of a living organism was science fiction. Now, we know it’s doable.”
Related Stories
- Two FDA-approved cancer drugs significantly reverse Alzheimer’s disease
- Harvard study finds common virus triggers multiple sclerosis in 97% of cases
From Science Fiction to Real-World Science
The work was carried out by a collaboration between JAX’s Rare Disease Translational Center (RDTC), the Broad Institute, and the nonprofit RARE Hope. Together, they brought expertise in genetics, disease modeling, and patient advocacy to a project that has been years in the making.
Cathleen Lutz, vice president of the RDTC and a leader of the study, helped develop the mouse models that made this research possible. These mice were engineered to carry the same mutations found in children with AHC, offering a rare chance to test treatments in an animal model that closely reflects human disease. For Lutz, the goal reaches beyond AHC. She sees this as a proof of concept that could apply to many rare conditions. “The idea of correcting mutations before someone ever develops symptoms is compelling,” she said. “But it requires the tools to do just that.”
Nina Frost, founder of RARE Hope and a co-author of the study, played a key role in aligning the science with real-world patient needs. As a parent of a child with AHC, she worked to ensure the research focused on what matters most to families. “Up until this point, we didn't know if this was a disease that could be rescued postnatally,” Frost said. “To see data that showed not just molecular correction in cells, but a functional rescue in mouse behavior, was an incredibly exciting moment.”
A Platform for Other Genetic Diseases
The potential impact goes far beyond AHC. About 80% of rare diseases are genetic. Many are caused by a single error in a person’s DNA, called a monogenic mutation. With the right tools, these errors could be corrected at the source.
In this study, researchers compared two methods: prime editing and traditional gene therapy. The latter involves adding new copies of a healthy gene. But for conditions like AHC, that approach may not work well because the faulty gene still produces a harmful protein. Prime editing, developed in 2019 by David Liu at the Broad Institute, offers a more direct fix. It doesn’t just add a copy—it rewrites the gene itself. And in this study, it worked better than gene therapy, especially in delicate brain cells.
“We’re not working with a patient at this point,” Terrey said, “but if we can do it for one gene variant—and we already have five in the paper—we can reasonably assume that we can do this for other variants as well.”
One of the major obstacles in gene editing for neurological disease is the brain’s natural defense system, called the blood-brain barrier. This protective layer makes it very difficult for substances, including treatments, to enter the brain. The researchers overcame this by using the AAV9 virus, which is able to pass through this barrier in newborn mice.
“The level of editing efficiency in the brain is really quite remarkable,” Lutz said. This opens the door to potential therapies for a wide range of brain disorders that were once seen as impossible to treat.
Gene Editing at the Start of Life
Delivering the treatment soon after birth proved to be key. The editing tools were able to reach many neurons while the brain was still developing. This early window gave the mice the best chance of avoiding severe symptoms later on. But scientists are now testing whether gene editing can help even after symptoms appear. This would be a game-changer for children who are diagnosed later or already experiencing problems.
“We haven’t necessarily reversed the disease,” Lutz said. “But we’ve shown we can ease symptoms when treatment is given early. The money shot, which we’re working on now, is whether we can treat the disease after symptoms appear. If we can show benefit then, that’s a whole new level.”
The safety of the approach is also promising. When tested in patient-derived cells, the editing showed minimal off-target effects. This means the tool mostly fixed only the intended gene, reducing the risk of unwanted changes elsewhere in the genome.
Looking Ahead to Personalized Therapies
This success builds on recent advances in gene therapy, including a landmark case earlier this year where gene editing healed a baby with a rare liver condition called CPS1 deficiency. That breakthrough showed it was possible to treat severe genetic disease in infants. Now, the ability to apply that same precision to the brain is taking the science even further.
Lutz leads the NIH Somatic Cell Genome Editing Consortium, a national effort to explore and expand gene editing. Her long-standing work with Liu, who helped develop prime editing, continues to push the field forward. “This study is an important milestone for prime editing,” Liu said. “It opens the door to one day repairing the genetic causes of many neurological disorders that have long been considered untreatable.”
The road ahead will involve more testing, including long-term safety studies and the search for the best timing and delivery methods. But the path forward is clearer than ever. By correcting the DNA inside brain cells, researchers are not just managing symptoms—they are rewriting the story of genetic disease.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.