Israeli scientists to perform the world’s first human spinal cord transplant surgery
Tel Aviv University is preparing the first human spinal cord implant trial, offering hope for people paralyzed by injury.
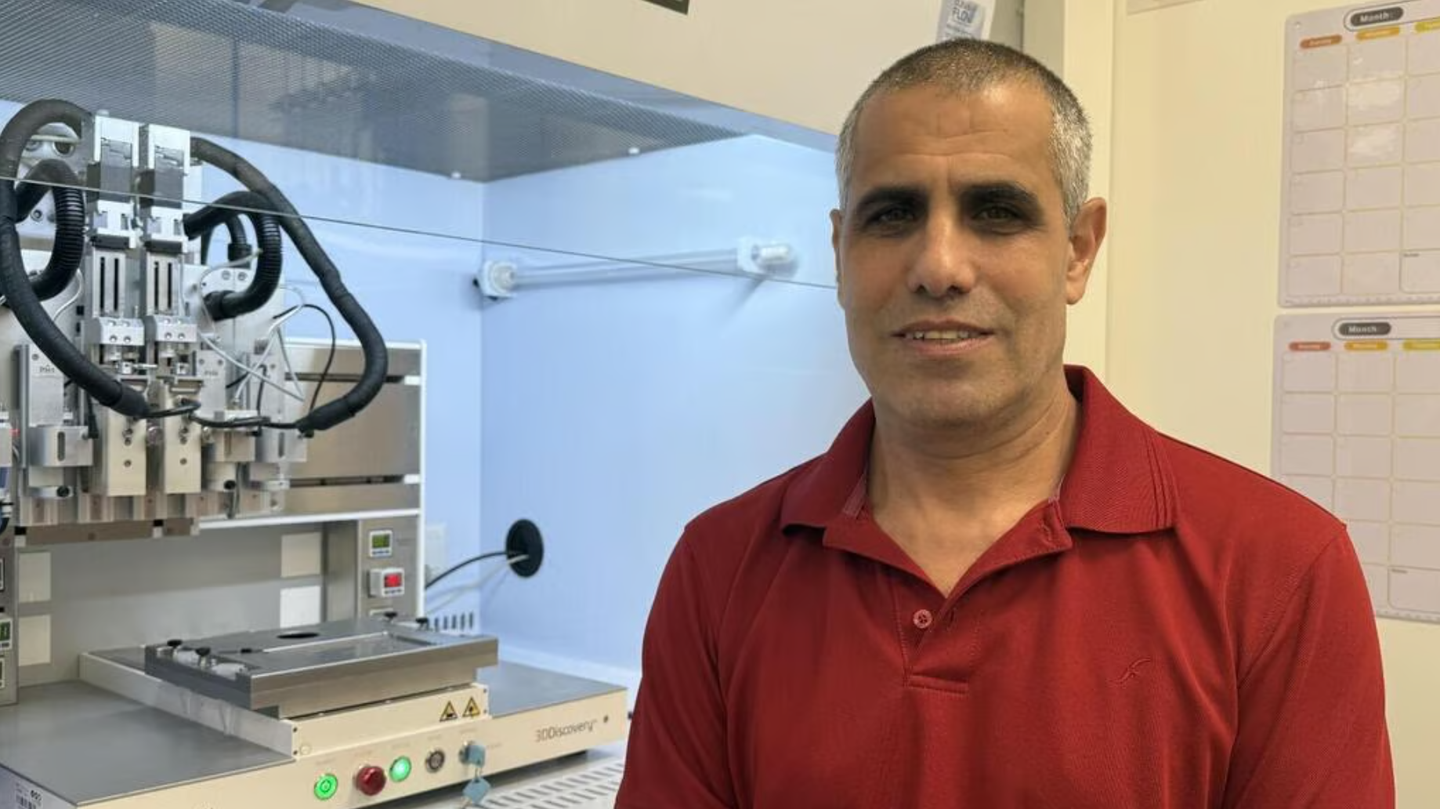
Prof. Tal Dvir says the first recipient of the new technology will be Israeli. (CREDIT: Matricelf)
For generations, paralysis from a damaged spinal cord has been seen as permanent. Once the nerves were injured, the signals carrying movement from the brain to the body were lost forever.
But scientists at Tel Aviv University believe they may have found a way to change that. Their research has produced a lab-grown spinal cord implant that could help people who can no longer walk regain movement. The world’s first human trials are now scheduled for this year.
Rebuilding the Body’s Electrical Cable
The spinal cord acts like a highway of electrical signals, moving instructions from the brain to every muscle. When trauma from a car crash, fall, or even a battlefield injury tears that cord, it’s as if an electrical wire has been cut. “If the two parts don’t touch, the electrical signal can’t pass,” explained Prof. Tal Dvir, head of Tel Aviv University’s Sagol Center for Regenerative Biotechnology. “The cable won’t carry electricity, and in the same way, the person can’t transmit the signal beyond the site of the injury.”
Unlike skin, which can heal itself, neurons don’t regenerate naturally. Once they’re damaged, the body can’t make new ones. That grim reality has left millions of people worldwide with no way back from paralysis. According to the World Health Organization, more than 15 million people live with spinal cord injuries today, most from traumatic accidents.
A Personalized Solution
To tackle the challenge, Dvir’s team designed a process that creates implants from a patient’s own cells. A small blood sample is reprogrammed into cells that behave like stem cells, capable of turning into any tissue type. At the same time, belly fat tissue is collected and broken down into substances such as collagen and sugars. These ingredients are used to make a personalized hydrogel.
This gel acts as the framework for the spinal cord implant. Scientists place the reprogrammed cells inside it and mimic the same processes that occur during embryonic development. The result is not just individual neurons, but a three-dimensional network of nerve cells that can transmit electrical signals. After about a month in the lab, the implant is ready to be placed into the damaged spinal cord.
Related Stories
- Breakthrough protein activates body's ability to heal spinal cord damage
- Breakthrough deep brain stimulation therapy restores walking after spinal cord injury
Success in Animal Models
When the team tested their approach in lab animals, the results were striking. “We showed that we can treat animals with chronic injuries. Not animals that were injured just recently, but those we allowed enough time to pass — like a person more than a year after an injury. More than 80% of the animals regained full walking ability,” Dvir said. In models with recent paralysis, the success rate reached nearly 100%.
This achievement marked the first time engineered human spinal cord tissue had restored movement in an animal with long-term paralysis. Recovery was rapid too. After rehabilitation, the animals were walking with surprising ease, offering hope that a similar result might one day be possible in people.
From the Lab to the Clinic
Encouraged by the animal data, the researchers submitted their findings to Israel’s Ministry of Health. Within six months, they received preliminary approval to begin compassionate-use trials with eight patients. The first surgery will take place in Israel.
“This is undoubtedly a matter of national pride,” Dvir said. “The technology was developed here in Israel, at Tel Aviv University and at Matricelf, and from the very beginning it was clear to us that the first-ever surgery would be performed in Israel, with an Israeli patient.”
For now, the initial focus will be on patients whose paralysis is relatively recent — within the past year. Once safety and effectiveness are proven, the hope is to expand treatment to those with long-standing injuries.
Building a Bridge Between Science and Industry
Behind this initiative is a collaboration between academic scientists and a young biotech company. In 2019, Dvir co-founded Matricelf with Dr. Alon Sinai to bring these engineered tissues into medical practice. The company’s CEO, Gil Hakim, has overseen the push toward regulatory approval, while Dr. Tamar Harel-Adar and her research team have driven the scientific development.
“They managed to get us to the stage of regulatory approvals so quickly — and that’s amazing,” Dvir noted. Hakim added: “This milestone marks the shift from pioneering research to patient treatment. Our approach, using each patient’s own cells to engineer a new spinal cord, eliminates key safety risks and positions Matricelf at the forefront of regenerative medicine.”
A Historic First Step
The first human implant is expected within a year. If successful, this would represent a new standard of care for spinal cord injuries, a condition that until now has had no cure. For many patients, treatments today involve only stabilizing the injury and preventing further damage. Surgery and rehabilitation can help maintain function but cannot restore what was lost.
With this new technology, researchers hope to move beyond maintenance and into true repair. “Our goal is to produce personalized spinal cord implants for every paralyzed person, enabling regeneration of the damaged tissue with no risk of rejection,” said Dvir. The journey ahead is filled with uncertainty, but also with promise. For the first time, walking again may no longer be out of reach.
Practical Implications of the Research
If the implants work as they did in animals, this therapy could change the lives of millions living with paralysis. It would mean moving from lifelong disability to regaining independence. The use of each patient’s own cells reduces the risk of rejection, opening the door for safer and more effective treatments.
On a larger scale, the approach could reshape regenerative medicine by proving that complex tissues can be rebuilt and successfully implanted. Beyond spinal injuries, the same technology may eventually be adapted to repair other parts of the nervous system, such as in stroke or degenerative diseases.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.