New pig-skin corneal implant restores vision to the blind
New pig-skin corneal implant restores sight to blind patients, offering a safe, affordable alternative to donor transplants.
Scientists have created a bioengineered pig-skin corneal implant that restored sight in blind patients. (CREDIT: Thor Balkhed)
Losing your eyesight to corneal disease can feel like an irreversible sentence, but scientists and entrepreneurs may have found a way to change that. A new implant, created from purified collagen protein derived from pig skin, has restored vision in people who were once blind.
The work, published in Nature Biotechnology and led by researchers at Linköping University in Sweden together with the company LinkoCare Life Sciences AB, could transform the future of eye care.
A Global Shortage of Donor Corneas
Corneal blindness affects an estimated 12.7 million people worldwide. The cornea is the clear outer layer of the eye that helps focus light, and when it becomes diseased or damaged, vision can be severely impaired or lost altogether. Today, the only treatment for advanced cases is a corneal transplant from a deceased human donor. But donor tissue is scarce—only one in 70 patients receives a transplant—and access to surgery is limited, especially in low- and middle-income countries where the need is highest.
That shortage inspired scientists to look for another solution. “The results show that it is possible to develop a biomaterial that meets all the criteria for being used as human implants, which can be mass-produced and stored up to two years and thereby reach even more people with vision problems,” explained Neil Lagali, professor at Linköping University’s Department of Biomedical and Clinical Sciences.
Building a Bioengineered Cornea
The research team designed a bioengineered cornea called BPCDX. To make it, they used highly purified collagen molecules taken from pig skin, a byproduct of the food industry. Pig tissue has long been used safely in medical products such as heart valves, making it a practical and affordable choice.
The collagen molecules were stabilized with a special crosslinking process that transformed them into a strong, transparent material that looks and behaves much like a natural human cornea. Unlike donated corneas, which must be transplanted within two weeks, these implants remain viable for up to two years when stored properly—making them far more accessible in regions without advanced eye banks.
Related Stories
- Scientists create 3D-printed eyes that look and feel like the real thing
- Breakthrough eye drops reverse vision loss from age-related macular degeneration
Mehrdad Rafat, adjunct associate professor at Linköping University and founder of LinkoCare Life Sciences AB, led the implant’s design and development. “We’ve made significant efforts to ensure that our invention will be widely available and affordable by all and not just by the wealthy,” he said. “That’s why this technology can be used in all parts of the world.”
A Gentler Way to Perform Surgery
Alongside the implant, researchers also developed a new surgical method designed to be less invasive than conventional corneal transplants. Traditionally, a patient’s diseased cornea is removed entirely and replaced with donor tissue that must be stitched in place—a complex operation usually performed only at specialized hospitals.
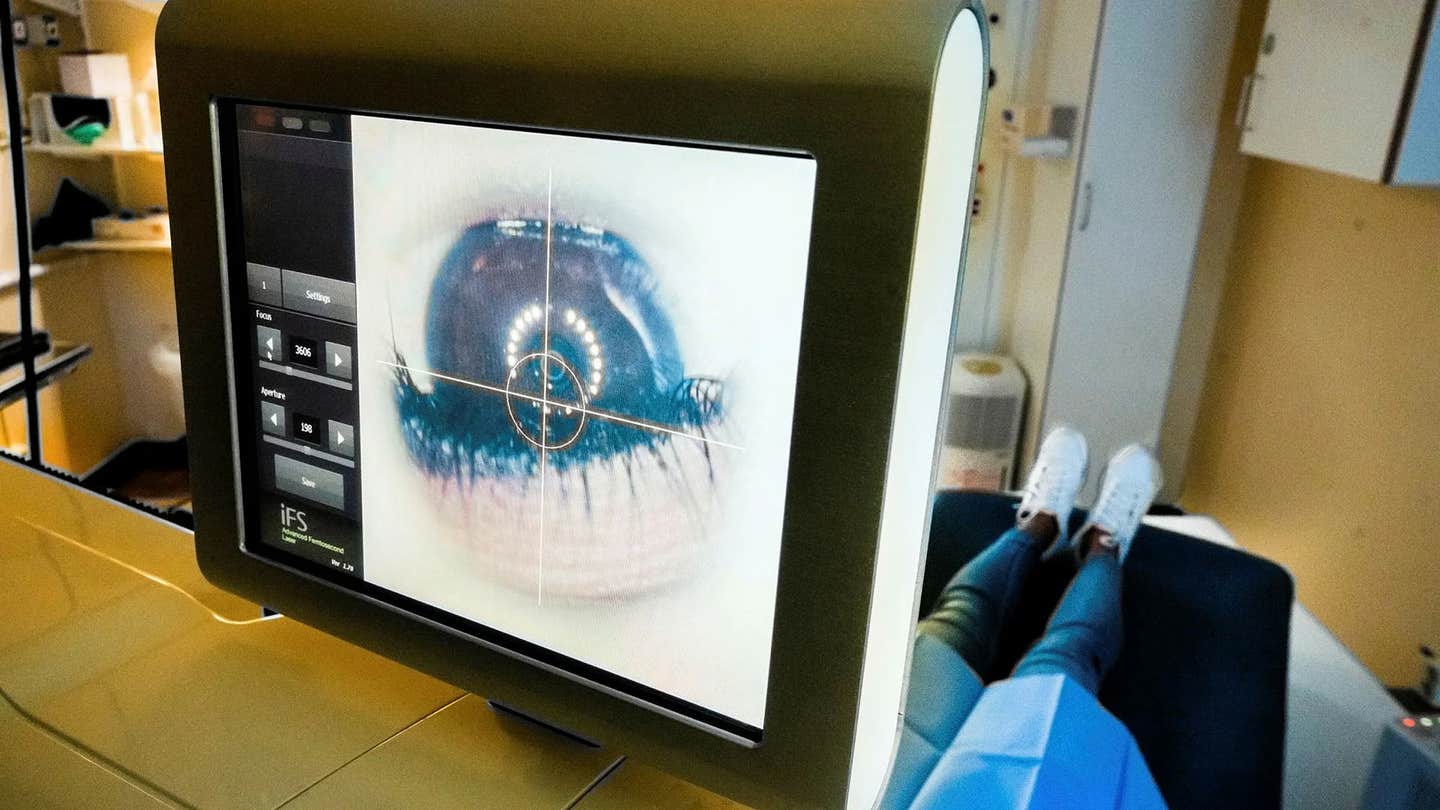
The new approach is simpler. Instead of removing tissue, surgeons create a small pocket within the patient’s existing cornea and slide the implant into place. No stitches are required, and the procedure can be done with high precision using a laser or even by hand with standard instruments.
“A less invasive method could be used in more hospitals, thereby helping more people,” said Lagali. “With our method, the surgeon doesn’t need to remove the patient’s own tissue.”
From the Lab to Human Eyes
Before testing in humans, the implant underwent extensive safety checks. Laboratory studies confirmed it caused no irritation or toxicity, while storage tests showed it remained stable and transparent over long periods. It was then tested in rats and mini-pigs to confirm safety and durability before advancing to human trials.
The first pilot study involved 20 patients in India and Iran with advanced keratoconus, a condition where the cornea becomes dangerously thin and misshapen. Many of the patients were blind or close to losing their vision completely.
The results exceeded expectations. Not only did the implants restore the normal thickness and curvature of the cornea, but they also improved sight dramatically. Before surgery, 14 of the 20 participants were blind. Two years later, none of them remained blind, and some regained perfect 20/20 vision. Three patients in India who had been unable to see clearly at all could now see as sharply as someone with healthy eyes.
Importantly, the surgeries had no complications. The tissue healed quickly, and patients only needed immunosuppressive eye drops for eight weeks to prevent rejection. In comparison, traditional corneal transplant patients must take such medications for years.
Why This Breakthrough Matters
For millions of people, this innovation could mean the difference between a lifetime of darkness and the chance to see again. The implant eliminates the need for donor corneas, reduces the risks associated with transplantation, and makes surgery possible in places that lack specialized hospitals.
The pilot study showed that the bioengineered cornea worked as well as donor tissue and offered additional advantages such as easier handling, longer storage, and faster recovery. The researchers are now preparing for larger clinical trials in Europe and beyond to confirm the results and move toward regulatory approval.
Practical Implications of the Research
If successful on a larger scale, these bioengineered corneal implants could make sight-restoring surgery accessible to millions who are currently left untreated. People in developing nations, where donor corneas are rarely available, stand to benefit the most. The technology’s affordability and long shelf life mean that hospitals in remote regions could stock implants and perform surgeries without relying on donor banks.
In the future, scientists also hope to adapt the implant for treating other eye diseases and even customize it for individual patients to maximize effectiveness. For families and communities affected by preventable blindness, this research offers not only restored sight but also restored independence, opportunity, and quality of life.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.