New research links changes in walking patterns to early Alzheimer’s
Changes in how you walk—especially how long each step is—may help flag early signs of Alzheimer’s or other brain-related conditions.

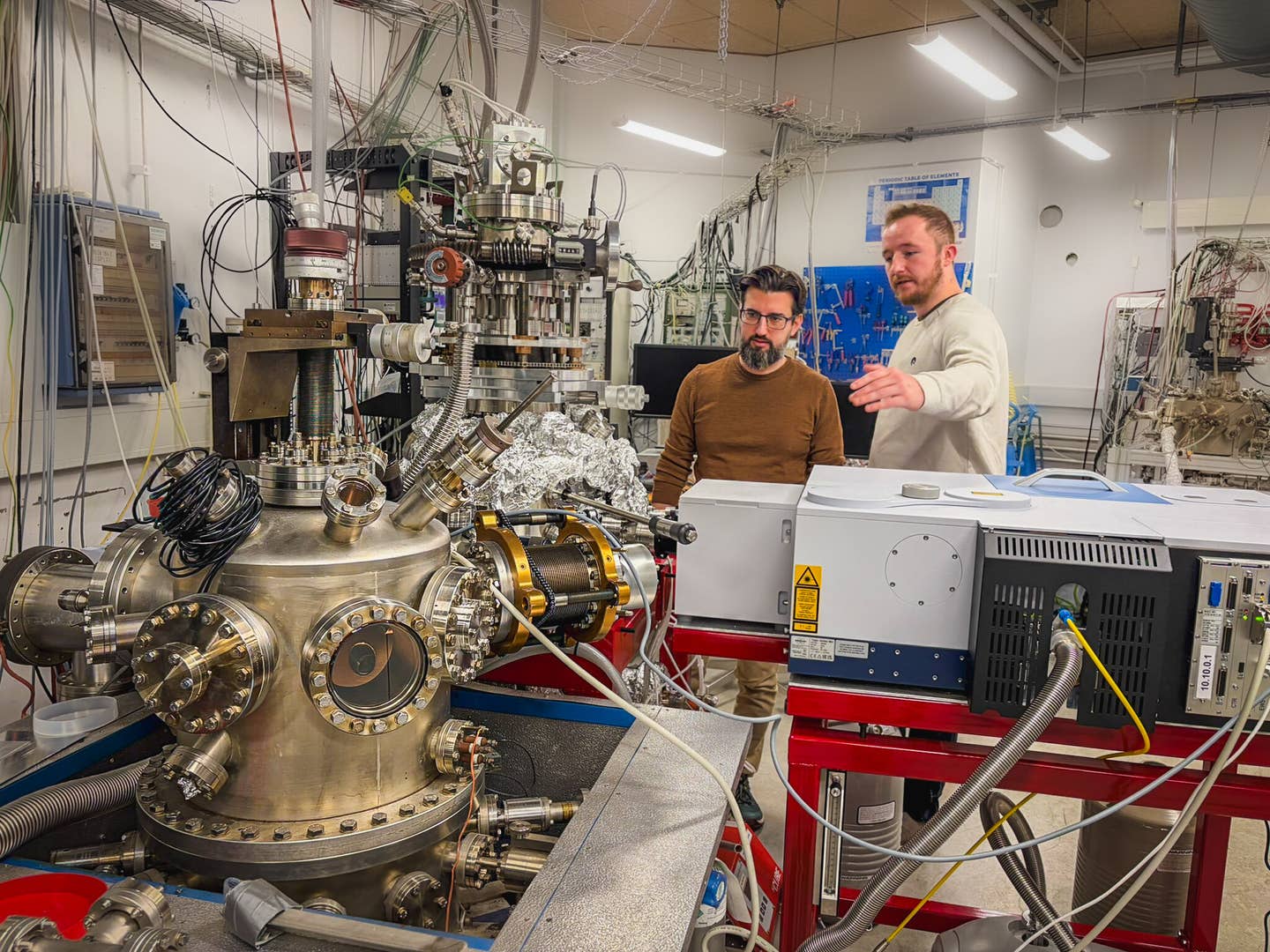
Alzheimer risk: This model can be integrated into a wearable device, attached to the lower back, for continuous monitoring of steps in daily life. (CREDIT: CC BY-SA 4.0)
Your steps could say more about your brain than you think. A new study shows that changes in how you walk—especially how long each step is—may help flag early signs of Alzheimer's or other brain-related conditions.
Researchers from Tel Aviv University and Ichilov’s Tel Aviv Sourasky Medical Center have developed a machine learning model that measures step length with pinpoint accuracy. This system, recently detailed in Digital Medicine, uses a small wearable sensor worn on the lower back. Unlike older tools found only in clinics, this new approach allows continuous monitoring during daily life.
“Step length is a sensitive indicator for various conditions, from cognitive decline to Parkinson’s disease,” the team explained. They noted that traditional systems are bulky and limited to specialized labs. The wearable device now offers precise data collection without disrupting a person’s routine.
The international team behind the work included researchers from Israel, Belgium, the UK, Italy, the Netherlands, and the U.S. It was led by Assaf Zadka, Prof. Jeffrey Hausdorff, and Prof. Neta Rabin. “Current methods give only short glimpses of walking behavior,” said Hausdorff. “But walking changes depending on fatigue, medication, and mood. We need to see what happens across an entire day.”
To do this, the team turned to IMU (inertial measurement unit) technology—found in devices like smartphones and smartwatches. These small sensors track movement with high precision and were key to solving the limitations of past systems. Prof. Rabin, an expert in machine learning, emphasized that even phone-based data could reveal higher chances of illness before other symptoms appear.
Unlike earlier IMU studies that only used healthy people, this new work aimed to include individuals with existing walking issues. The challenge was to make the device not only accurate but also comfortable enough to wear all day. That way, it could capture step patterns in familiar, everyday settings—like the walk to the fridge or mailbox.
Related Stories
By combining real-world motion data with artificial intelligence, the team has moved one step closer to better screening for neurological decline. With further testing, the system may help spot issues before the brain begins to fail, offering a clearer path toward earlier diagnosis and care.
To develop the algorithm, the researchers used IMU sensor-based gait data and conventional step length data from 472 subjects with various conditions, including Alzheimer's, Parkinson's, mild cognitive impairment, multiple sclerosis, and healthy individuals. This generated a diverse database of 83,569 steps.
The team employed machine learning to train models that translated IMU data into step length estimates. To test the models' robustness, they assessed their ability to analyze new data accurately.
"The XGBoost model proved the most accurate, being 3.5 times more precise than the current advanced biomechanical model," said Zadka. "For a single step, our model's average error was 6 cm, compared to 21 cm for the conventional model. Evaluating an average of 10 steps, the error dropped to less than 5 cm, a clinically significant threshold."
The study's findings suggest the model's reliability and potential for real-world application. "Our model is robust and reliable, suitable for analyzing sensor data from subjects with walking difficulties who weren't part of the original training set," Zadka concluded.
This research marks a significant advancement in non-invasive monitoring of neurological conditions, offering a practical and accurate method to track and potentially predict the progression of diseases like Alzheimer's and Parkinson's.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.