New study reveals why some cells are more susceptible to cancer than others
Slower-dividing cells resist cancer, even with mutations. New study uncovers cell cycle speed as key to cancer prevention.
A new study finds that how fast cells divide may determine whether cancer develops, offering hope for new prevention therapies. (CREDIT: CC BY-SA 4.0)
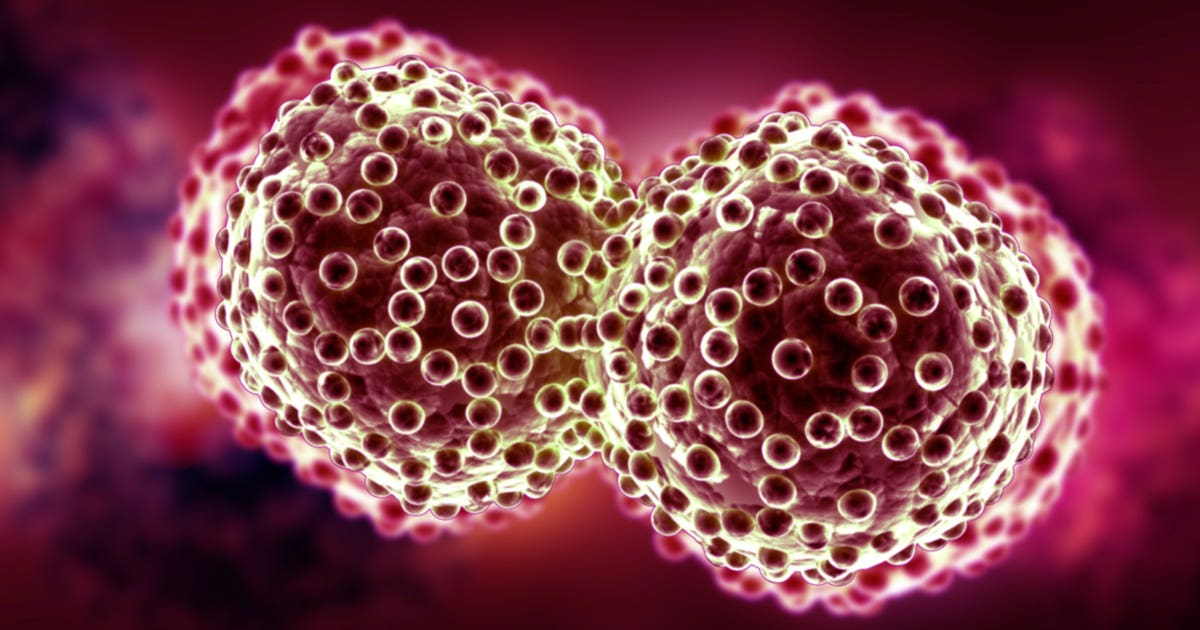
A hidden clue may explain why some mutated cells become cancerous and others don’t: how fast they divide.
A new study from researchers at Sinai Health in Toronto reveals that the total time it takes for a cell to complete one full cycle of division—called the total cell cycle duration, or Tc—can predict whether it will develop into a tumor. Faster-dividing cells are more likely to turn cancerous, while slower ones often escape this fate.
This discovery adds a new layer to what scientists know about cancer and its origins. It suggests that simply having cancer-causing mutations isn’t enough. How a cell responds to that mutation—and especially how quickly it divides—plays a key role in whether it will eventually become a tumor.
Cancer Without a Cause?
Cells in your body collect mutations throughout your life. These genetic errors can happen for many reasons: environmental exposure, inherited traits, or random mistakes during cell division. But surprisingly, most mutated cells never become cancer.
Dr. Rod Bremner, Senior Investigator at Sinai Health’s Lunenfeld-Tanenbaum Research Institute, explains it this way: “An average adult has millions and millions of cells which have mutations in them, yet thankfully, we don’t develop cancer all the time.”
His team wanted to understand why. If mutations alone don’t trigger cancer, what does?
To find out, they started by studying retinoblastoma, a rare eye cancer found mostly in children. Researchers looked at cells that had mutations in the Rb gene—a well-known tumor suppressor. This gene normally controls how and when cells divide.
Interestingly, mice with mutated Rb genes didn’t develop tumors in most tissues, even though the cells were dividing in unusual ways. In fact, when Rb-deficient embryonic stem cells were introduced into early-stage embryos, those cells ended up in nearly every adult tissue. But only the pituitary gland developed tumors. The rest of the cells stayed normal despite having dangerous mutations.
Related Stories
This raised a critical question: What makes some cells give in to cancer and others resist, even with the same genetic error?
Speed Matters More Than You Think
Dr. Bremner and his colleague, Dr. Danian Chen, decided to look at the rate at which cells divide. The team introduced different mutations known to cause cancer in a range of tissues—like the lung, retina, and pituitary gland. They found something striking.
In every case, the cancer developed from the cell type with the shortest cell cycle. That is, the fastest-dividing cells were the ones most likely to turn cancerous.
This pattern held true for various genetic mutations. For instance, the combination of Rb and p53 loss caused tumors in fast-dividing neuroendocrine lung cells. Other mutations like KrasG12D and BrafV600E triggered tumors in alveolar type 2 cells, which also have short Tc values.
Even in tissues with different kinds of mutations, the link was the same: shorter cycle time meant higher risk.
Further analysis showed that extending Tc—slowing down the division rate—prevented tumors from forming. And this suppression happened even when typical defenses like immune clearance or programmed cell death didn’t activate.
In one model, blocking a specific pathway in the SKP2–p27–CDK2/CDK1 axis stopped cancer from developing. This approach didn’t affect other features of the cells, like their ability to undergo apoptosis or immune detection. It worked purely by changing the pace of division.
Normal Cells, Not Dead Ones
This research challenges the idea that only cell death or immune surveillance keeps cancer in check. In fact, many of the body’s mutated cells don’t die—they just stop dividing abnormally and behave like normal cells.
“The most common way that mutated cells escape cancer is just by becoming normal cells,” said Dr. Bremner. “They divide abnormally a little bit and then they stop and look like any other normal cell.”
In other words, not every mutated cell triggers an immune response or self-destructs. Most simply return to normal growth patterns, especially if their division pace is slow enough to avoid dangerous buildup.
This helps explain why people don’t constantly develop tumors, even though their tissues are full of cells carrying cancer-associated mutations.
Rethinking Cancer’s Origins
For years, scientists have studied the hallmarks of cancer—traits that almost all tumors share, like uncontrolled growth, resistance to death, and the ability to attract blood vessels. But the new findings suggest there’s another hallmark worth adding: total cell cycle duration.
It’s not just what mutations are present that matters. It’s also how the cell behaves afterward. A faster cycle appears to be a key ingredient in the mix that leads to cancer.
The researchers also emphasized that Tc can identify the “cell of origin” for various cancers—the original cell that turned malignant. In all models tested, the cell with the shortest cycle turned into cancer, even when different mutations were introduced at different times.
This could help scientists understand where specific cancers start and why some cells are more vulnerable than others.
A New Path for Prevention?
The most exciting part of this work is its potential for new treatment strategies. If slowing down cell division can keep tumors from forming, then future therapies could aim to adjust Tc in high-risk individuals.
“Our work suggests that we might be able to intervene in cancer-prone cells to slow them down a little bit with the right therapeutic agents,” said Dr. Bremner. “But first, we need to understand the mechanisms governing cell cycle rate in different cell types.”
The research hints that one day, treatments could focus on enhancing the natural resistance that most cells already show. Instead of killing cancer cells, doctors could stop tumors from forming in the first place—just by giving cells a little more time between divisions.
There’s still much to learn. But these findings offer a fresh way to think about cancer—one that focuses not just on genetics, but on timing.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.