New weekly injectable drug could transform the lives of people living with Parkinson’s disease
Scientists develop a weekly injectable for Parkinson’s that could replace daily pills and improve drug delivery and quality of life.
A new weekly injectable developed in Australia could replace daily pills for Parkinson’s disease, offering stable relief with fewer side effects. (CREDIT: ABC News / Guido Salazar)
A new weekly injection may soon transform how millions manage Parkinson’s disease. For over 8.5 million people living with this condition worldwide, daily treatment has meant taking levodopa and carbidopa tablets several times a day. These frequent doses help ease symptoms like tremors, stiffness, and slow movement. But for elderly patients and those with difficulty swallowing, this schedule is difficult to follow and can lead to inconsistent relief.
Now, researchers at the University of South Australia (UniSA) have created a long-acting injectable that could simplify this routine into a once-a-week dose. Their new formulation, reported in the journal Drug Delivery and Translational Research, combines science, safety, and ease into a single, slow-releasing implant.
A weekly injection that releases medication steadily
The new injectable contains levodopa and carbidopa—key drugs used to treat Parkinson’s symptoms. Once injected under the skin or into muscle, the biodegradable gel steadily releases both drugs over seven days. This slow and consistent release helps keep drug levels stable in the blood, reducing side effects linked to drug peaks and valleys.
Lead researcher Professor Sanjay Garg, from UniSA’s Centre for Pharmaceutical Innovation, says this could revolutionize Parkinson’s care. “Our goal was to create a formulation that simplifies treatment, improves patient compliance, and maintains consistent therapeutic levels of medication,” he said. “This weekly injection could be a game-changer.”
Levodopa has long been the gold standard for Parkinson’s. It crosses the blood-brain barrier and turns into dopamine, a chemical that becomes scarce in Parkinson’s. But its short half-life means patients must take it multiple times each day. This can lead to fluctuations in symptom control and increase the risk of non-compliance.
Carbidopa is added to help. It stops levodopa from breaking down too soon in the body. This makes more of the drug available to reach the brain, reducing side effects like nausea and improving effectiveness.
Related Stories
A closer look at how the system works
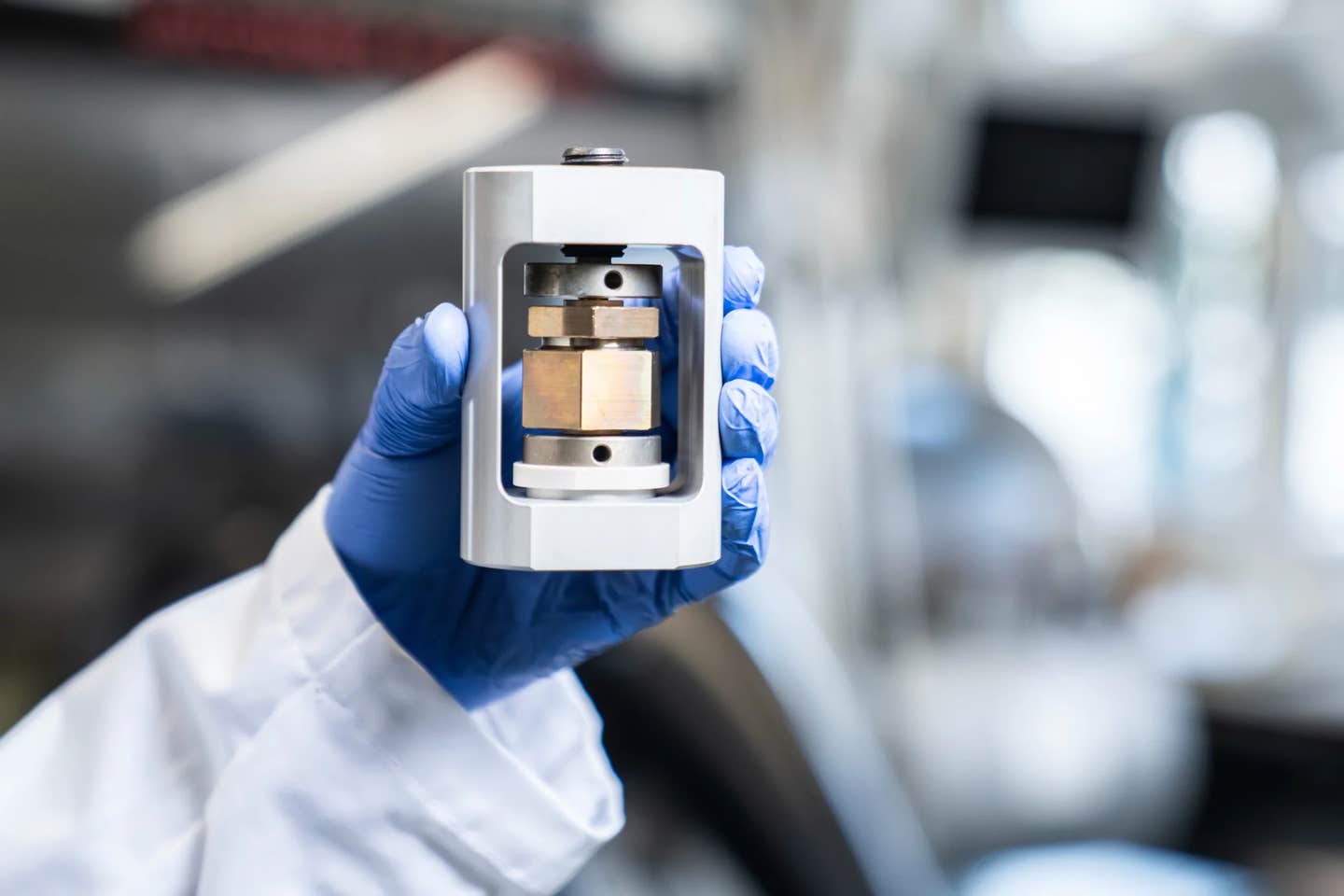
The injectable system uses a mix of PLGA (poly-lactic-co-glycolic acid), a well-known FDA-approved biodegradable polymer, and Eudragit L-100, a pH-sensitive polymer. When injected, the solution forms an implant inside the body, slowly releasing the drug without needing surgery to insert or remove it.
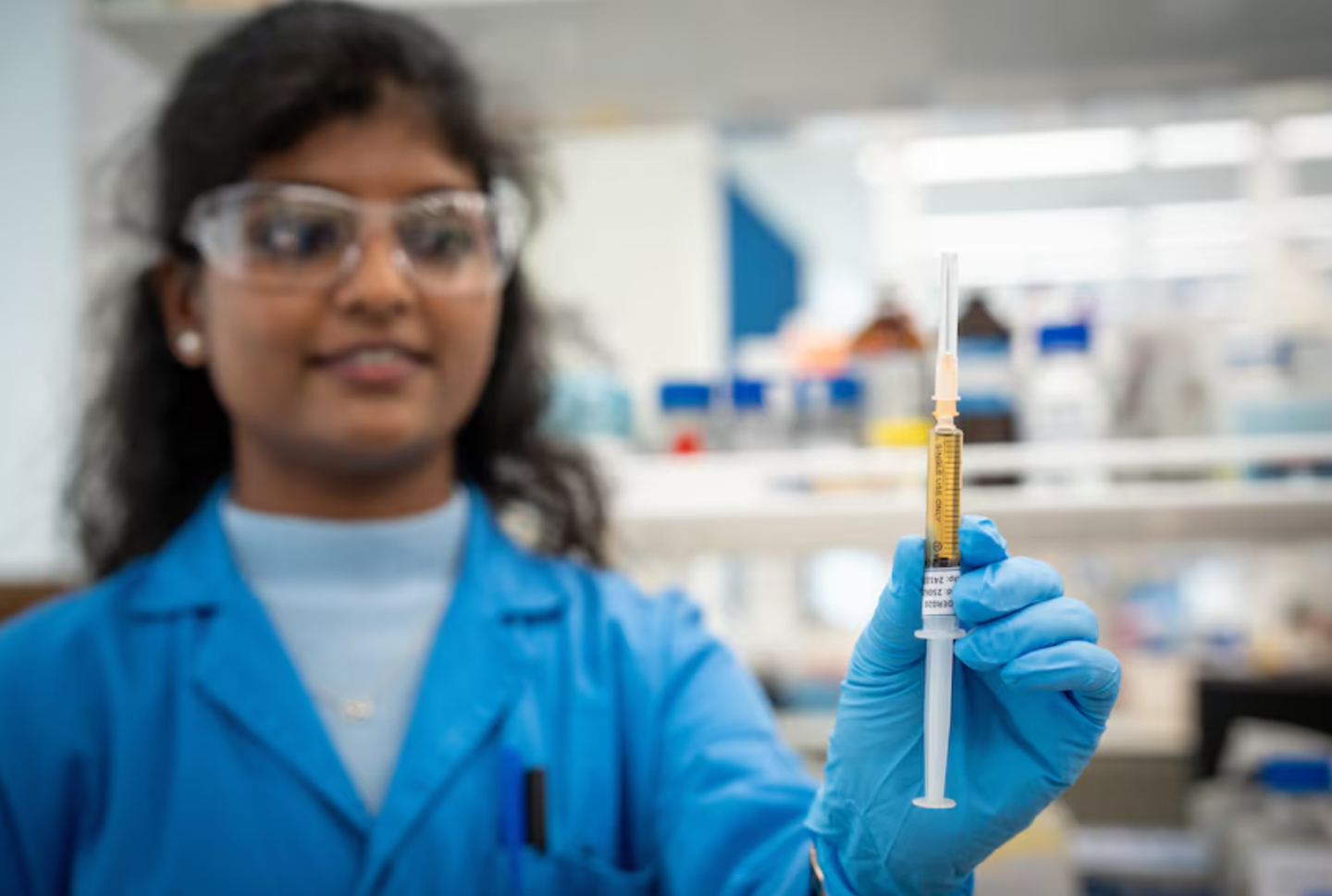
UniSA PhD student Deepa Nakmode says the design was years in the making. “After years of focused research, it's incredibly rewarding to see our innovation in long-acting injectables for Parkinson’s disease reach this stage. Our invention has now been filed for an Australian patent,” she said.
The optimized formula includes 26% PLGA and 6% Eudragit L-100. Lab studies showed that over seven days, more than 90% of the levodopa and 81% of the carbidopa were released. During the first 24 hours, about one-third of the drugs were released, which helps achieve fast symptom relief early on.
Tests also showed the implant broke down by over 80% in one week. Importantly, there was no sign of toxicity in cell tests, and the injection could be given using a standard 22-gauge needle, making it painless and easy for most patients.
Solving problems with current treatments
Parkinson’s is a progressive brain disorder caused by the loss of dopamine-producing neurons. While there’s no cure, current treatments aim to reduce symptoms. The most common is oral medication. But this comes with downsides: frequent dosing, uneven drug levels, and a high chance of missed doses.
Earlier versions of extended-release tablets helped some patients, but they didn’t fully solve the problem. They couldn’t completely stop the highs and lows in drug levels, and they still required at least daily administration.
This new injectable addresses that need by maintaining consistent drug release, improving convenience and potentially enhancing quality of life. “By reducing the frequency of dosing from multiple times a day to a weekly injection is a major step forward in Parkinson’s therapy,” Prof Garg said. “We’re not just improving how the drug is delivered; we’re improving patients’ lives.”
Why in-situ implants stand out
Long-acting injectables have gained popularity in chronic disease treatment because they improve patient compliance and reduce side effects. In-situ forming implants offer unique benefits compared to other systems like solid implants or microspheres.
Unlike solid implants, which may need surgery to insert or remove, in-situ implants are injected as a liquid that solidifies inside the body. This method avoids the need for high temperatures, added ions, or surgery. It works by solvent exchange: after injection, the body’s fluids interact with the implant, causing the polymers to harden and release the drug slowly.
PLGA was chosen for this study because it’s widely used in drug delivery due to its safety and flexibility. It breaks down naturally in the body and allows scientists to fine-tune how fast it dissolves. The team used a 50:50 mix of lactic and glycolic acid with a low molecular weight, which ensures faster breakdown—ideal for a weekly release.
Adding Eudragit L-100 improved the control over how the drug is released. This pH-sensitive polymer dissolves at pH 6 or higher, which is suitable for muscle or subcutaneous injection. The team tested various ratios of PLGA and Eudragit to achieve the right balance between release rate and injectability. One formulation, labeled P5, stood out.
Tests showed the final product had a smooth viscosity, behaved like a Newtonian fluid (meaning it flows evenly), and required only about 33 newtons of force to inject. That’s well within range for common clinical practice.
Strong lab results and next steps
The researchers used both lab tests and computational modeling to study the drug’s performance. They predicted a peak drug level (Cmax) of 399.3 nanograms per milliliter at 24 hours, with a total drug exposure (AUC) of 26,505.5 ng/mL over an infinite time horizon. These results suggest a reliable release of the drug throughout the week, assuming full bioavailability.
The gel system holds several advantages. It delivers high doses without surgery, avoids large needle requirements, and is easy to produce. These benefits make it suitable not just for Parkinson’s but also for other long-term conditions that need regular medication, such as diabetes, cancer, chronic pain, and infections.
Next, the UniSA team plans to start human trials and is exploring partnerships to bring the product to market. If successful, it could replace multiple daily pills with a weekly injection and open the door to new forms of drug delivery in neurology and beyond.
A broader future for long-acting injectables
The field of long-acting injectables has expanded in recent years. Drug companies have tested various delivery systems, including oily suspensions, liposomes, microneedles, and implants. But in-situ implants remain especially promising because they allow for larger drug loads, tunable release, and simpler administration.
Previous research focused mostly on microspheres and solid implants, which had limits like low drug loading, inconsistent dispersion, and the need for removal. In-situ systems avoid many of these problems and provide a cleaner, more user-friendly solution. Several commercial products already use similar methods, including Atridox and Eligard.
The formulation created by UniSA may soon join that list, offering new hope for people who struggle with the burdens of daily medication.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.