Scientists destroy cancer cells with LED light and tin nanoflakes
Tin nanoflakes and LED light create a safe, low-cost cancer therapy that kills tumor cells while sparing healthy tissue.
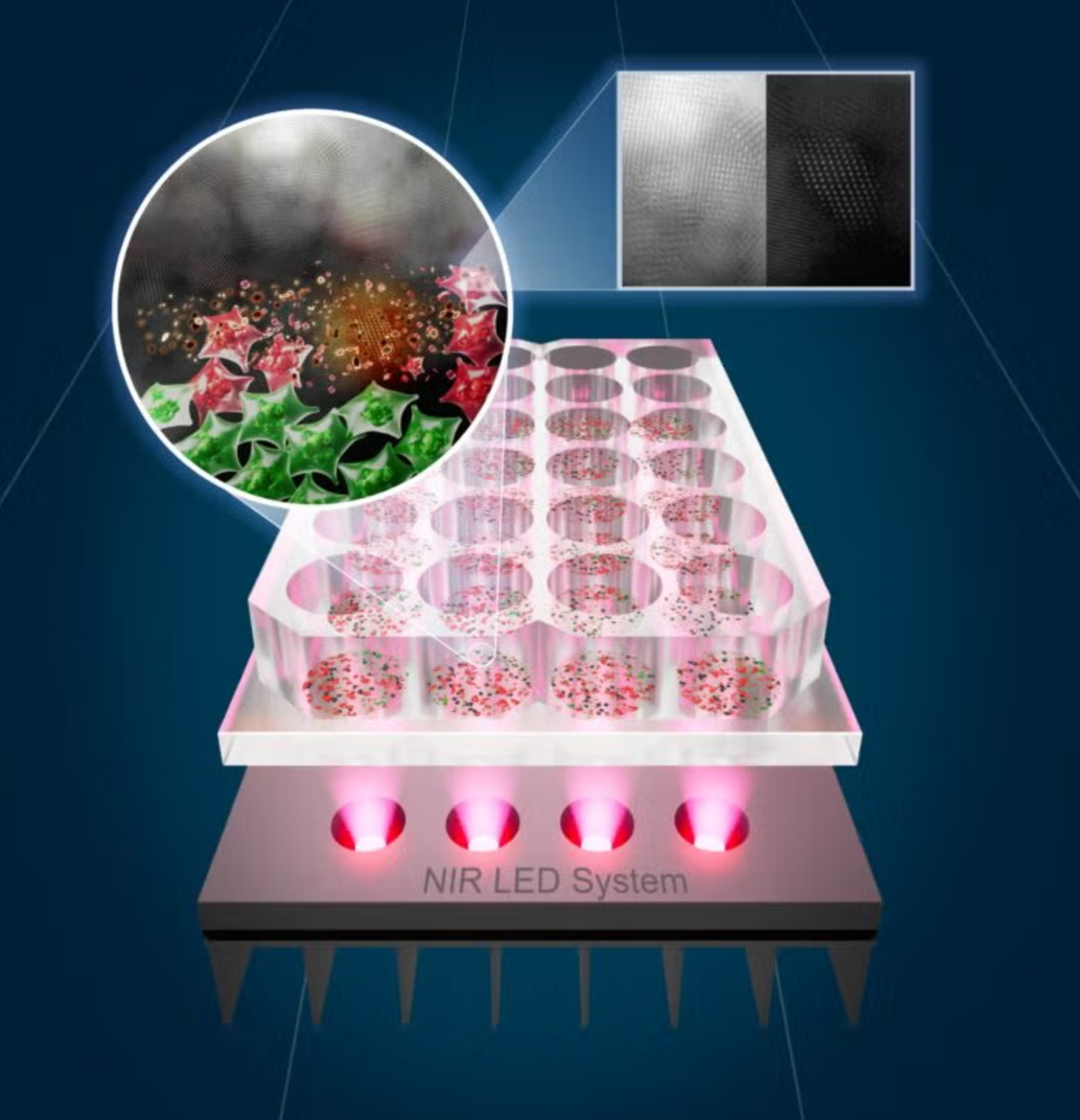
he researchers’ custom near-infrared LED heating system activates SnOx nanoflakes that heat and neutralize cancer cells (green: live cells; red: cells killed by photothermal therapy). (CREDIT: UT Austin)
A team of researchers at The University of Texas at Austin and the University of Porto have created a new way to target cancer—tin-based nanomaterials combined with near-infrared light. Their work has the potential to result in less toxic, cheaper cancer treatments that are light-based rather than violent drugs or radiation.
The key lies in small tin oxide nanoflakes, or SnOx, which are fabricated through a simple electrochemical process that transforms tin disulfide (SnS₂) into a new structure. The nanoflakes absorb near-infrared (NIR) light and convert it to heat that kills cancer cells but spares the healthy ones. The photothermal therapy exactly attacks the tumors by causing heat wherever light is concentrated.
Jean Anne Incorvia, a professor at UT Austin's Cockrell School of Engineering, said that the goal was to have the treatment be "effective and accessible." The scientists have discovered a way to bypass the use of costly lasers that can also harm surrounding tissue by combining LED light with tin nanoflakes.
Converting Tin into a Cancer Killer
The researchers began with layered SnS₂ nanosheets, which they electrochemically oxidized to SnOx nanoflakes. That introduced tiny imperfections called oxygen vacancies—essential defects that allow the material to absorb more light and emit more heat.
Electron microscopy found that the oxidized flakes were thinner and more porous than their predecessors, with a higher surface area to interact with light. That structure, added to the novel chemical composition, made them very effective at converting light into heat.
They rapidly heated up water solutions to above 60°C, a temperature that is lethal for killing cancer cells when nanoflakes of iron oxide were irradiated with NIR at 808 nanometers—the wavelength optimal for penetration of deep tissue. They had a photothermal conversion efficiency of 45.6%, significantly higher than that of the control material.
Safe, Targeted, Reusable
In tests, cancer cells exposed to the nanoflakes were not highly toxic when they were not exposed to light, i.e., the particles are not toxic in dark. But when exposed to NIR light, they proved fatal for cancer cells. In tests on colorectal and skin cancer cells, a 30-minute treatment killed up to 92% of skin cancer cells and half of the colorectal cancer cells. Healthy human skin cells remained unaffected.
Fluorescence microscopy revealed the nanoflakes invading cancer cells and diffusing through their cytoplasm. When excited, the flakes emit bursts of heat spikes that break through membranes and cause apoptosis—cell death—without damaging surrounding tissue.
The materials were also proof against prolonged use. Even when subjected to a number of heat and cool cycles, their structure and function remained stable. In water storage, they did not clump and retained their optical characteristics for a prolonged period, making them stable enough for use in medicine.
LEDs Instead of Lasers
One of the major breakthroughs in this study was substituting expensive, high-power lasers with light-emitting diodes. LEDs provide a cheaper and safer source of energy, making treatment easier to scale and safer for clinic use.
"It's our aspiration to bring this technology to patients worldwide," stated Artur Pinto, a scientist at the University of Porto and co-senior author on the study. He hopes for a handheld LED device for skin cancer that patients might apply in their own homes following surgery. The tiny patch-like device would provide site-specific light treatment to kill any remaining cancer cells and reduce the risk of recurrence.
This move toward LED-based therapy would drive light-based treatments into hospitals, or indeed homes, particularly in areas where large equipment is not available.
The Science Behind the Glow
The secret to the nanoflakes' success is oxygen vacancies—tiny spaces in the atomic lattice that change how the material reacts to light. Vacancies create new electronic states that have an increased range of NIR wavelengths to absorb, and thus better photon capture and heat generation.
Computer modeling confirmed that the oxidized tin oxide has a lower bandgap, so it takes in more light energy and releases it as heat instead of reflected light. This synergy of nanostructure design and defect engineering combines the material to be both efficient and versatile. Researchers can even customize its response by adjusting oxidation conditions.
In contrast with other photothermal materials, such as gold nanorods or carbon materials, SnOx nanoflakes are very low cost, chemically stable, and eco-friendly with fabrication. The entire process is conducted at room temperature without any toxic chemicals, posing a green and scalable method to medical nanomaterial fabrication.
Looking Ahead
The researchers want to investigate the nanoflakes further by testing them in live animal models to observe how they circulate in the body and determine long-term safety. They are also exploring ways to blend the particles with other materials used as catalysts so that they can be applied more broadly to medicine.
The technology has applications well beyond cancer. The same light-activated heat could be used in antimicrobial therapy or wound healing, where focused heat accelerates recovery.
As Incorvia neatly summarized, "This is a step towards light-based medicine that's not only powerful but practical."
Practical Implications of the Research
The SnOx nanoflakes can be a breakthrough in treating cancer by offering a noninvasive, targeted, and cheap alternative therapy. The combination of LED light and tin nanoflakes will make photothermal therapy safer and more accessible to hospitals and clinics worldwide.
Porterables could later bring post-surgery light therapy into patients' home living rooms, particularly for surface cancers such as melanoma.
The research would contribute to ensuring that cancer treatment is bearable to patients using lesser use of chemotherapy and radiation; it is less expensive and less demanding on infrastructure. It truly offers hope to patients in advanced and resource-poor health systems.
Research findings are available online in the journal ACS Nano.
Related Stories
- Scientists re-engineer a patient’s own T cells to target and destroy cancer cells
- Cambridge scientists reprogram brain cancer cells to stop them from spreading
- Breakthrough therapy forces cancer cells to self-destruct
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Mac Oliveau
Writer
Mac Oliveau is a Los Angeles–based science and technology journalist for The Brighter Side of News, an online publication focused on uplifting, transformative stories from around the globe. Passionate about spotlighting groundbreaking discoveries and innovations, Mac covers a broad spectrum of topics including medical breakthroughs, health and green tech. With a talent for making complex science clear and compelling, they connect readers to the advancements shaping a brighter, more hopeful future.



