Scientists identify two enzymes driving memory loss in Alzheimer’s disease
New study finds SIRT2 enzyme drives GABA overproduction in Alzheimer’s, opening new paths for targeted memory loss treatment.

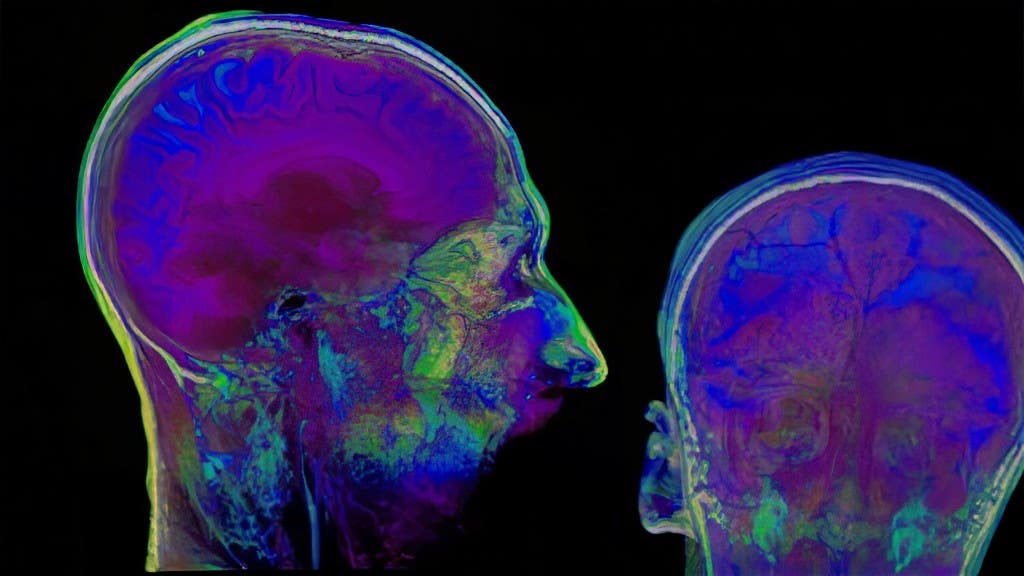
A breakthrough study has uncovered the role of the SIRT2 enzyme in Alzheimer’s, showing how astrocytes may fuel memory loss and brain decline. (CREDIT: CC BY-SA 4.0)
For many years, astrocytes were seen as simple support cells in the brain. Today, that picture is changing fast. These star-shaped brain cells do more than provide structural help—they actively shape how the brain works. In the case of Alzheimer’s disease, astrocytes undergo major changes that may be worsening the condition.
Alzheimer’s is known for its buildup of sticky amyloid-beta plaques, which are harmful protein clumps that damage brain cells. When astrocytes detect these plaques, they spring into action. They attempt to break them down using internal processes like autophagy and the urea cycle. While these processes can help remove plaques, they also spark unintended side effects.
As they try to clean up the brain, astrocytes produce too much GABA, a chemical messenger that slows down brain activity. This overflow of GABA causes memory problems and weakens communication between neurons. At the same time, astrocytes also release hydrogen peroxide (H₂O₂), a toxic compound that leads to further brain damage.
A new study by researchers at the Institute for Basic Science sheds light on why this happens—and offers a possible way forward.
Led by Director C. Justin Lee of the IBS Center for Cognition and Sociality, a team of scientists has identified two key enzymes behind this problem: SIRT2 and ALDH1A1. These enzymes are part of the chemical pathway that turns a molecule called putrescine into GABA. While the early part of this pathway was already known, the steps that came after were a mystery—until now.
Using a mix of advanced lab techniques—such as molecular imaging, gene analysis, and brain scans—the team found that both SIRT2 and ALDH1A1 were elevated in the brains of people with Alzheimer’s, as well as in mice genetically engineered to mimic the disease.
SIRT2, in particular, was found in large amounts in astrocytes located in the hippocampus, the brain region tied to memory. When researchers blocked the gene that produces SIRT2 in these mice, they saw a decrease in GABA levels and a small return of short-term memory abilities. However, not all types of memory improved.
Related Stories
“When we inhibited the astrocytic expression of SIRT2 in AD mice, we observed partial recovery of memory and reduced GABA production,” said Mridula Bhalla, lead author of the study. “While we expected reduced GABA release, we found that only short-term working memory (Y-maze) of the mice was recovered, and spatial memory (NPR) was not. This was exciting but also left us with more questions.”
This suggests that SIRT2 is only one part of a larger picture. Blocking it doesn’t stop the brain damage entirely. It only slows one part of the decline.
What makes this discovery so important is that it opens the door to more precise treatments. Until now, Alzheimer’s drug research has mostly focused on MAOB inhibitors—drugs that block the early part of the same pathway. These drugs reduce both GABA and hydrogen peroxide, but that creates a problem: it becomes impossible to know which chemical is doing the most damage.
Director Lee explained why that matters: “So far, we have been using MAOB inhibitors in AD research, which block the production of H₂O₂ as well as GABA. By identifying enzymes SIRT2 and ALDH1A1 downstream to MAOB, we can now selectively inhibit GABA production without affecting H₂O₂, which would allow us to dissect the effects of GABA and H₂O₂ and study their individual roles in disease progression.”
In simple terms, targeting SIRT2 lets researchers control GABA levels without touching hydrogen peroxide. This helps them better understand which compound is responsible for different symptoms in Alzheimer’s.
One key finding from the study was that even when SIRT2 was blocked and GABA levels fell, hydrogen peroxide continued to be released. That means brain cell damage can still occur. According to Director Lee, “inhibition of SIRT2 continued H₂O₂ production, indicating that neuronal degeneration might continue even though GABA production is reduced.”
This makes clear that both GABA and hydrogen peroxide have their own roles in the disease, and both need to be studied separately.
While this discovery is a big step forward, it’s not a cure. SIRT2 may not be a direct drug target because it doesn’t stop the full process of neurodegeneration. But it does offer a valuable research tool.
This enzyme can now be used to untangle how each chemical—GABA and hydrogen peroxide—contributes to memory loss, confusion, and brain cell death. With this knowledge, scientists may be able to build more focused treatments that avoid unwanted side effects.
The study also revealed that ALDH1A1 plays a role in the same pathway, though its influence appears more limited than SIRT2’s. Still, identifying both enzymes fills a crucial gap in understanding how astrocytes drive brain decline.
By linking these enzymes to reactive astrocytes, the study shows how changes in brain support cells can have wide-reaching effects. Once thought of as passive helpers, astrocytes are now taking center stage in Alzheimer’s research.
Alzheimer’s disease remains one of the most devastating conditions in the world. More than 55 million people globally live with dementia, and Alzheimer’s accounts for 60% to 70% of those cases. Despite decades of research, progress has been slow.
This new study, published in Molecular Neurodegeneration, stands out for its detailed approach and sharp focus on a lesser-known part of the brain’s chemistry. With an impact factor of 15.1, the journal is highly respected in neuroscience.
By shifting the spotlight to astrocytes and the enzymes they use, this research offers fresh hope. It doesn’t promise a miracle drug. But it does bring scientists one step closer to understanding how Alzheimer’s works—starting at the cellular level.
New treatments may one day come from studies like this. If future drugs can fine-tune the chemical output of astrocytes without harming other cells, then more effective and safer options could be possible.
What matters now is that scientists can finally study the damaging effects of GABA and hydrogen peroxide on their own. That’s a major step toward solving the puzzle of memory loss and brain aging.
As Director Lee put it, the real value here lies in precision. With better tools, researchers can ask better questions—and eventually, find better answers.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.