Stanford scientists use ultrasound to deliver drugs with fewer side effects
Stanford scientists use sugar and ultrasound to guide drugs with pinpoint accuracy, offering safer, targeted treatments.
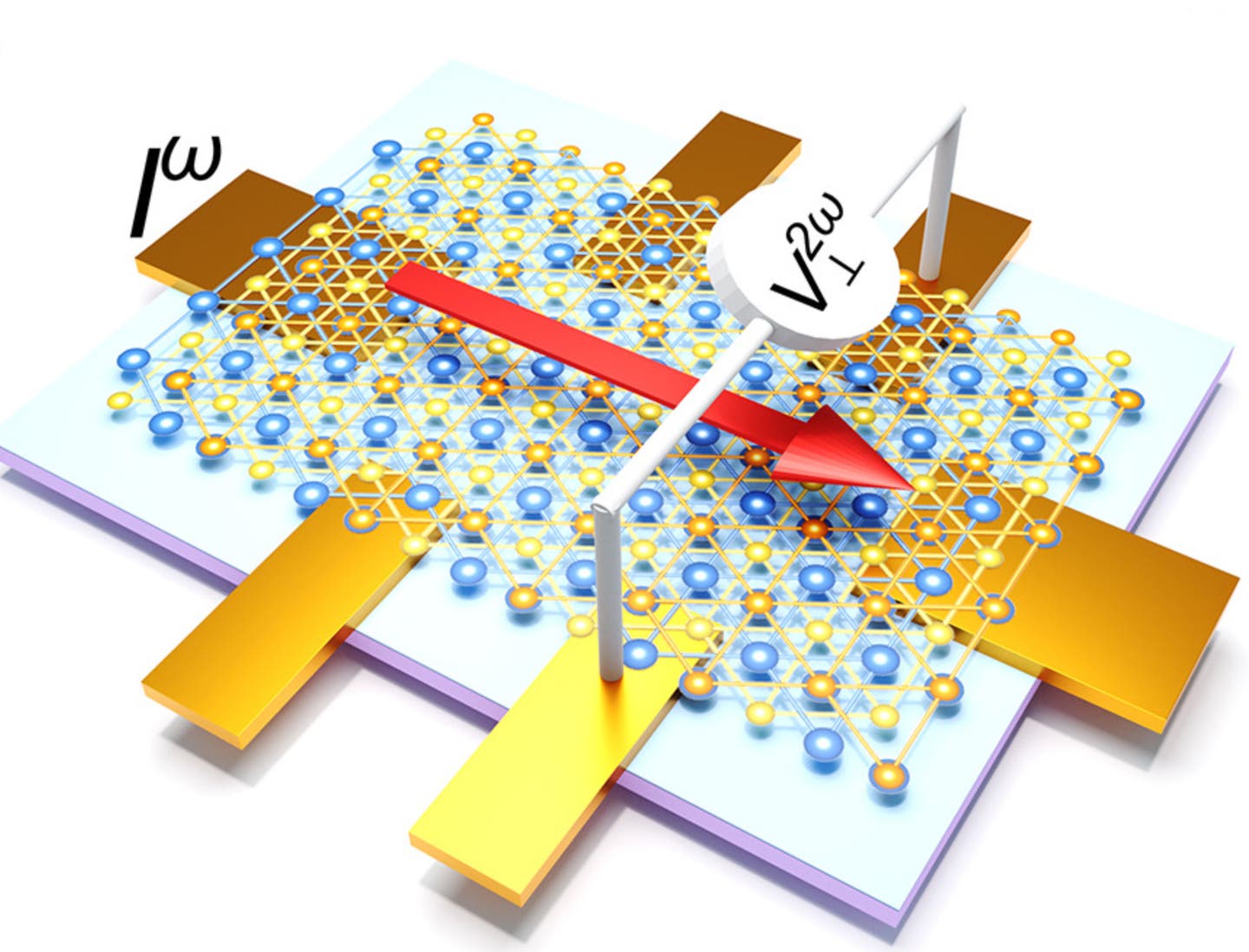
Stanford researchers created sugar-filled nanoparticles that release drugs with ultrasound. (CREDIT: AI-generated / The Brighter Side of News)
When medicines go to the wrong places in the body, the results can be rough. Antidepressants may cause feelings of detachment, chemotherapy can harm healthy tissues, and painkillers often bring nausea. For years, scientists have searched for a way to get drugs precisely where they’re needed without hurting everything in their path. Now, a team at Stanford Medicine believes they’ve found a surprisingly simple solution: a little sugar and a touch of sound.
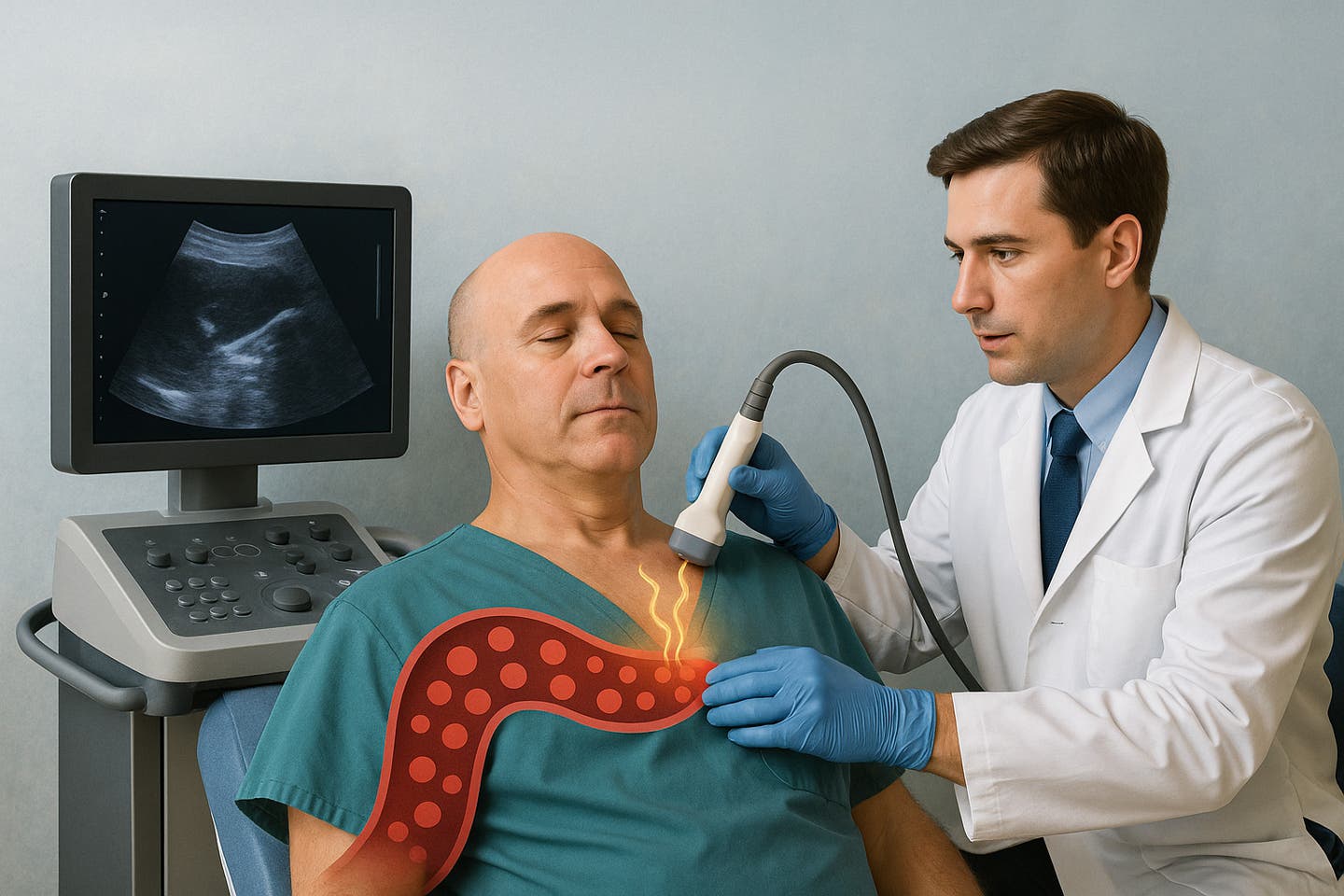
The method uses nanoparticles, tiny capsules that can carry drugs through the bloodstream, combined with carefully focused ultrasound. Together, they offer a system that can release medicine at a chosen site in the body with pinpoint accuracy—sometimes within just a few millimeters.
The latest version of this approach, described in Nature Nanotechnology, proved successful in rats, where it was used to send ketamine to specific regions of the brain and painkillers to individual nerves in the limbs.
A Safer, Simpler Design
What sets this method apart from earlier attempts is how stable and easy the nanoparticles are to make. The team switched from complex chemical shells to liposomes—small, bubble-like structures already widely used in medicine. You may know them as the same delivery system used for mRNA in COVID-19 vaccines.
The real twist was what went inside. Researchers discovered that filling the liposomes with a 5% sucrose solution made them just stable enough to circulate in the body but still responsive to ultrasound. When a narrow beam of ultrasound is aimed at a target, it vibrates the nanoparticles and releases the drug exactly where it’s needed.
“Turns out just a little bit of sugar is all you need to make this work,” said Dr. Raag Airan, assistant professor of radiology and senior author of the study.
Related Stories
- Ultrasound technology brings wireless power to medical implants
- Breakthrough ultrasound treatment painlessly eliminates kidney stones
This small addition made the system safer, easier to store, and more practical for everyday medical use. Unlike earlier versions that required unusual materials and freezing at extremely low temperatures, these sugar-loaded liposomes can be made using standard pharmaceutical processes and stored more easily.
The Road to Reinvention
Airan’s team has been chasing ultrasound-guided drug delivery for nearly a decade. Back in 2018, they showed it was possible to deliver the anesthetic propofol to a precise region in the rat brain. While promising, the technology wasn’t ready for patients. The polymer nanoparticles used back then were unstable, held little drug, and leaked at body temperature.
“The clinical translatability of that system was pretty limited,” Airan explained. “We had a real need to come up with something else, so we went back to the drawing board.”
The answer came partly from everyday cooking. Airan, while in the kitchen, wondered what could make the liquid inside the liposomes denser and more responsive to ultrasound waves. Sugar was the obvious candidate. Tests later confirmed that sucrose struck the perfect balance—dense enough to react with ultrasound but not so much that the drug would leak out on its own.
Targeting the Brain and Beyond
Once the sugar-based formulation was ready, the team tested it with ketamine in rats. They compared standard injections of free ketamine to ketamine sealed inside the liposomes. Without ultrasound, the rats that received the encapsulated drug had less than half the amount of ketamine in their organs compared with rats that received the free drug.
That meant the liposomes were keeping most of the medicine safely sealed. When ultrasound was directed at a specific region of the brain, however, about three times as much ketamine was released there compared to other brain areas.
The effect wasn’t just chemical—it was behavioral. Rats that received targeted ketamine to their medial prefrontal cortex, a brain region tied to emotional control, showed fewer signs of anxiety. They spent more time exploring the center of a box instead of hiding along the edges, a classic sign of reduced stress in animal studies.
“It’s not just that we’re getting the on-target effect,” Airan said. “We’re getting more of it than what you might expect, based on how much we’re delivering to that part of the brain.”
The hope is that if this works in humans, doctors might one day use ketamine to treat depression without triggering its disorienting side effects.
Easing Pain Without the Needle
The team also tested whether the system could be used for pain relief. They encapsulated ropivacaine, a common local anesthetic, and aimed ultrasound at the sciatic nerve in one leg of a rat. That leg quickly became numb to a prick test. A short ultrasound session of just two and a half minutes produced numbness that lasted an hour.
The benefit here is twofold. Not only does this provide targeted relief, but it also spares patients from needing painful injections at the exact site of discomfort. The drug can be injected somewhere less sensitive, while ultrasound does the work from outside the body.
Ready for Human Trials
The research team is now preparing for the first human trial, pending approval from the U.S. Food and Drug Administration. Their plan is to use ketamine delivered by this system to target the emotional aspects of chronic pain.
This time, Airan feels optimistic about wider adoption. Earlier prototypes used unusual chemicals that scared off pharmaceutical companies. Now, with common ingredients like sugar and lipids, the design is far more appealing.
“It’s eminently translatable,” Airan said.
Practical Implications of the Research
If this method proves successful in people, it could reshape how doctors treat many conditions. Psychiatric drugs could be delivered to brain regions linked to mood without affecting other areas. Painkillers might provide relief to a single limb or nerve without dulling the entire body. Even cancer therapies could one day be aimed directly at tumors, sparing healthy cells from toxic side effects.
For patients, this means safer treatments with fewer unwanted reactions. For doctors, it offers a flexible platform that could be adapted for many different drugs. And for the healthcare system, it promises more efficient use of medicine and possibly lower costs from reduced complications.
By pairing a common kitchen ingredient with an ultrasound wand, scientists may have unlocked a powerful new way to make medicine both smarter and safer.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.