Study finds BMI isn’t a reliable health tool after all
A new study reveals BMI fails to predict early death. Measuring body fat directly is more accurate, researchers say.

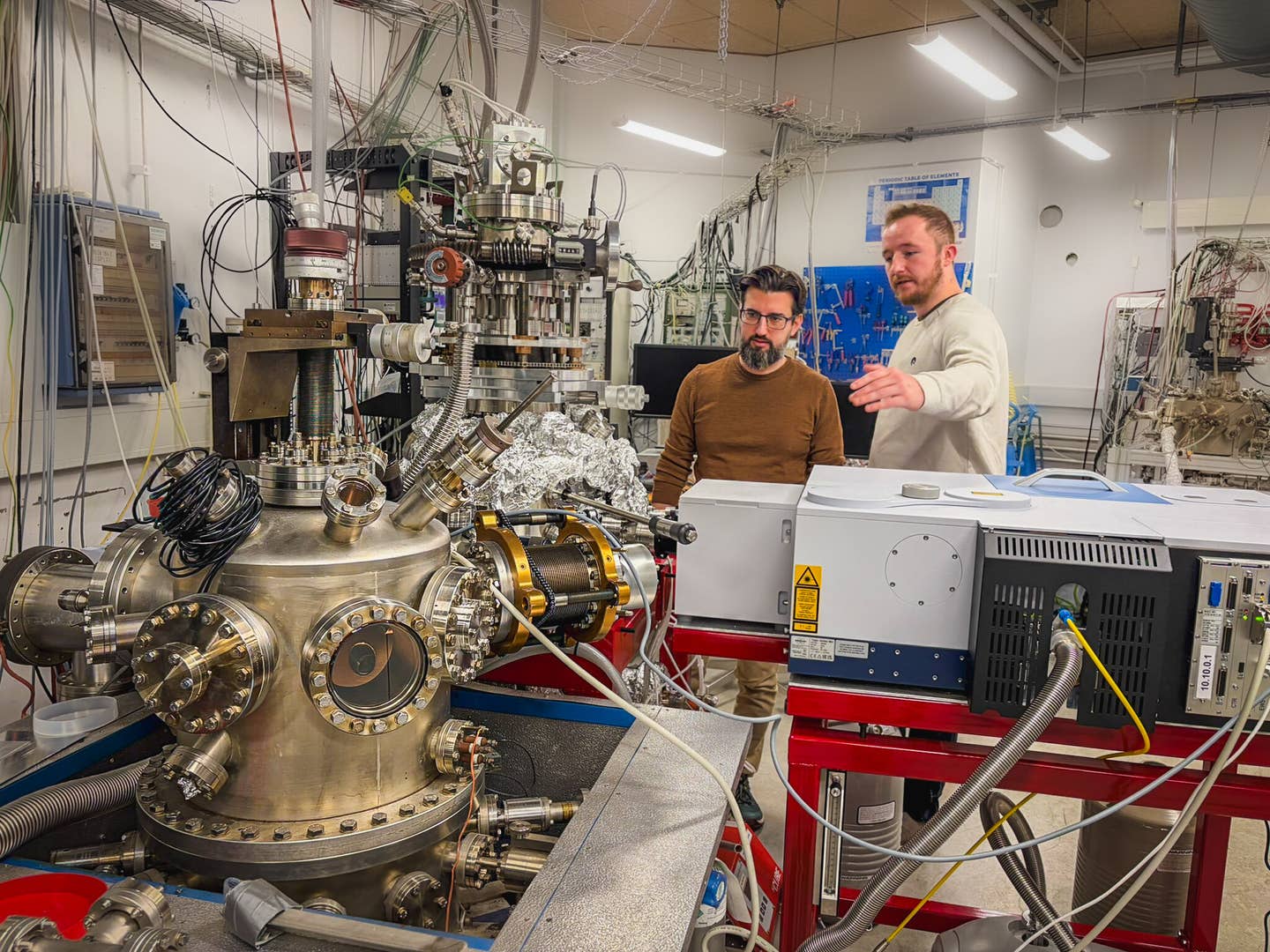
Researchers say a better, more direct way to measure body fat exists and should replace BMI in doctor’s offices everywhere. (CREDIT: Shutterstock)
A simple number has shaped how people think about health and weight for decades. That number is body mass index, or BMI. Doctors, schools, insurance companies, and even personal fitness apps have used it to classify people as underweight, normal, overweight, or obese. But new research shows BMI may not be telling the full story — and in many cases, it's telling the wrong one.
A new study from researchers at the University of Florida Health challenges the idea that BMI can predict future health risks. They found that BMI fails to accurately predict who is more likely to face weight-related health problems. Instead, they say a better, more direct way to measure body fat exists and should replace BMI in doctor’s offices everywhere.
What BMI Can’t Tell You About Your Health
BMI uses a person’s height and weight to place them into broad categories. The formula is simple: weight divided by height squared. But while it’s easy to calculate, it doesn’t show how much fat someone has or where that fat is stored.
That’s a big problem, according to the new study. The research tracked over 4,200 adults between ages 20 and 49 for 15 years. What they found should make doctors rethink how they assess health risks.
The people with high body fat — measured directly by a tool that sends a tiny electrical current through the body — had a 78% higher chance of dying from any cause within 15 years. Even more alarming, they were about three and a half times more likely to die from heart disease. This held true even after adjusting for other factors like age, race, and income.
Meanwhile, people who had high BMIs didn’t show a significantly greater risk of early death. In fact, BMI alone had no reliable link to 15-year mortality risk, even for heart disease.
“This is a game-changer,” said Arch Mainous, Ph.D., lead author of the study and a professor at the UF College of Medicine. “This is the ultimate Coke versus Pepsi test. And BMI failed.”
Related Stories
- Cutting ultra-processed foods doubles weight loss in new study
- New drug reduces both cholesterol levels and body weight, helping millions
A Better Way to Measure Body Fat
The more accurate method used in the study is called bioelectrical impedance analysis. It works by sending a low-level electrical current through the body. Because fat resists electricity more than muscle or water, the device can estimate how much body fat someone has.
These machines are now common in many medical offices, fitness centers, and even home scales. They’re fast, easy to use, and cost-effective. Unlike BMI, they provide a direct measurement of fat mass, not just weight.
The study’s data came from the National Health and Nutrition Examination Survey, a long-running national survey that collects health information from a broad cross-section of Americans. It also links that data to the national death index, allowing researchers to follow health outcomes over time. The findings remained clear: bioelectrical impedance gave a more reliable picture of who might face greater health risks down the road.
BMI: A Flawed Tool Still in Use
Despite its flaws, BMI is still widely used in doctor’s offices as a health “vital sign,” similar to blood pressure or heart rate. But many experts argue that needs to change.
“I’m a family physician, and on a regular basis, we’re faced with patients who have diabetes, heart disease, obesity and other conditions that are related to obesity,” said Frank Orlando, M.D., senior author of the study and medical director of UF Health Family Medicine – Springhill.
“One of the routine measures we take alongside traditional vital signs is BMI. We use BMI to sort of screen for a person having an issue with their body composition, but it’s not accurate for everyone like vital signs are.”
BMI doesn’t account for muscle mass, bone structure, or fat distribution. That means someone with a lot of muscle — like an athlete — might be labeled “obese” even if their body fat is low. On the other hand, someone with a normal BMI could still have high levels of body fat, especially around vital organs — the type of fat most strongly linked to disease and early death. These hidden risks aren’t captured by BMI, making it a poor tool for guiding treatment decisions.
Time for a Shift in How We Measure Health
The researchers behind the study are urging doctors and healthcare systems to move away from BMI. They believe bioelectrical impedance analysis offers a clearer, more accurate way to assess a person’s body composition and health risks.
This isn’t just a small tweak to how we view weight. It could change how we screen for disease, how we track progress in medical care, and even how insurance companies evaluate risk.
More than 4,200 adults in the study provide a strong signal: it’s not just about how much you weigh — it’s about how much fat you carry. And most importantly, where that fat sits in your body.
BMI may be fast and simple, but the science shows it doesn’t tell you what matters most. It’s time for a better tool — one that reflects the body more clearly and helps people understand their real health risks.
The Bottom Line
This study offers strong evidence that BMI has little value when predicting early death or heart problems. Directly measuring body fat gives a clearer view of health and should replace BMI as the standard.
As Dr. Mainous said, “This study is a game-changer.” And with better tools now widely available, there’s little reason to stick with a system that doesn’t work.
Research findings are available online in the journal The Annals of Family Medicine.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.