The future of surgery is learning from machines
AI systems are coaching medical students in surgery and could reshape health care and robotics in the years ahead.

 Edited By: Joseph Shavit
Edited By: Joseph Shavit

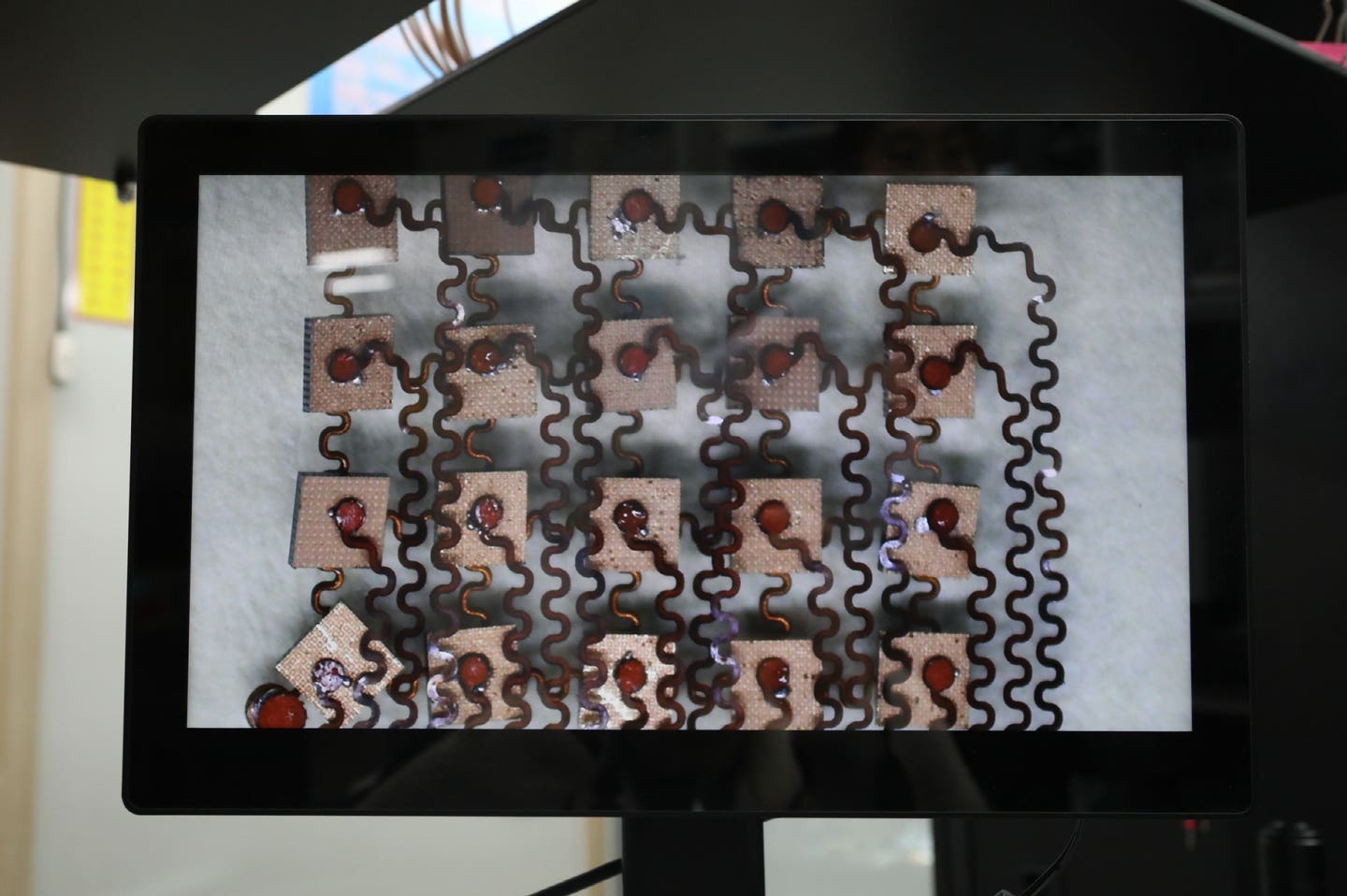
A Johns Hopkins AI tool now guides medical students during suturing practice, pointing to a future where robots and software reshape surgery and training. (CREDIT: Shutterstock)
A deep strain is running through hospitals around the country. There are not enough surgeons, and the shortage is growing. Long hours, rising burnout and years of training have made it harder to keep operating rooms fully staffed. Now, a quiet new helper is entering medical school labs, not in a white coat but in lines of code.
At Johns Hopkins University, researchers have built an artificial intelligence system that watches how doctors stitch wounds and then coaches students as they practice. It does not just judge performance. It explains what went wrong, what worked and how to improve the next move.
“We’re at a pivotal time. The provider shortage is ever increasing and we need to find new ways to provide more and better opportunities for practice,” said senior author Mathias Unberath, an expert in AI assisted medicine at Johns Hopkins. “The next best thing might be our explainable AI that shows students how their work deviates from expert surgeons.”
The system analyzes videos of skilled doctors closing incisions. It tracks their hand paths, speed and pressure. When students pick up a needle and try to repeat the task, the AI compares every motion to the expert record. Then it sends real-time guidance by text message, almost like a coach watching from just over your shoulder.
Currently, students learn mostly by watching videos and trying to copy what they see. Some programs use AI to score skill, but those systems cannot explain the score. Unberath said that leaves students wondering what to fix.
“These models can tell you if you have high or low skill, but they struggle with telling you why,” he said. “If we want to enable meaningful self-training, we need to help learners understand what they need to focus on and why.”
Lessons That Talk Back
The research team tested the system on 12 medical students who already had some experience with suturing. Half trained with AI guidance. The rest practiced by watching videos of surgeons. All students then stitched a second time.
Those with more experience who received AI advice improved much faster than students who only watched videos. Beginners still struggled, but those who already understood the basics took big steps forward.
“In some individuals, the AI feedback has a big effect,” Unberath said. “Students with a solid foundation in surgery, who are at the point where they can incorporate the advice, it had a great impact.”
First author Catalina Gomez, a computer science doctoral student at Johns Hopkins, said the system works because it gives direct, honest feedback.
“Learners want someone to tell them objectively how they did,” Gomez said. “We can calculate their performance before and after the intervention and see if they are moving closer to expert practice.”
The project received international praise and was honored at a recent major medical imaging conference. The team now wants to make the tool easier to use and cheap enough for students to try at home with a smartphone and a practice kit.
“We’d like to offer computer vision and AI technology that allows someone to practice in the comfort of their home,” Unberath said. “This is really about how can we use this technology to solve problems.”
A Shift Inside Medicine
This quiet breakthrough is part of a much larger shift inside health care. For decades, medicine has been split into two camps. Some doctors focus on diagnosing and managing disease. Others treat illness with tools and procedures. Over time, the second group rose in status and pay as technology made surgery faster and more powerful.
Now, that balance may be changing again.
Generative AI systems like ChatGPT have shown how machines can write, plan and explain at a high level. In medicine, similar systems are trained on textbooks, scientific papers and surgical recordings. They learn the patterns of how experts think and act.
Today, AI can already describe each step of a gallbladder operation. To perform surgery, however, it needs eyes and hands. That is where robotics enters the picture.
When Robots Become Surgical Partners
Modern surgical robots already give doctors better vision and steadier hands. A surgeon sits at a console and guides robotic arms inside the body. Cameras send back clear images. The movements are smooth and precise.
In the future, researchers believe generative AI could study thousands of recorded surgeries and learn to copy those same motions. Visual data from the camera would be matched with the gestures of expert hands. Over time, the system would learn what to do in response to what it sees.
The approach is not unlike the training of self-driving cars, but the operating room is more controlled than city streets. The human body changes less from person to person than traffic patterns.
Safety testing would be strict. Regulators could compare operations guided by AI with those done by surgeons, using anonymous videos. Approval would only come once the results looked the same.
Elon Musk has already predicted that the Tesla humanoid robot project called Optimus could one day perform advanced medical work. While that future is still uncertain, progress is moving quickly.
Training, Pay and Trust Will Change
Whether robots assist surgeons or take over certain tasks, the ripple effects will be wide. Residency programs may need to accept fewer surgical trainees while expanding training in primary care. Demand for chronic disease management is growing, and surgeon demand may eventually shrink.
Money systems will also have to adapt. Today’s hospitals make more when procedures take longer. A move toward bundled payments, one set price for an entire surgical episode, could reward safety and speed instead. Better control of disease could save trillions in health costs, according to federal estimates.
Cultural change may be the hardest part. Doctors rarely welcome tools that challenge tradition or income. Many patients will worry too. But history offers clues. Early fears about ATMs did not last. Over time, trust grew as reliability became clear.
Underserved communities could be among the first to accept AI driven tools. Once results prove safe, wider use is likely to follow.
Related Stories
- AI-powered robot learned to perform surgery by watching doctors work
- Cutting-edge AI technology reinvents surgery through real-time diagnoses
- A new kind of coach: How artificial intelligence is helping people prevent diabetes
Like these kind of feel good stories? Get The Brighter Side of News' newsletter.
Shy Cohen
Writer